Virtual reality improves surgical training, patient safety
Ophthalmic surgery requires microsurgical techniques to be executed with dexterity, precision and proficiency. Understandably, providing a risk-free environment to teach and practice microsurgical skills is challenging and is traditionally accomplished via microsurgical wet labs and highly supervised surgical procedures. Fortunately, surgical simulators have rapidly evolved in the last decade and are now being incorporated into many ophthalmology training programmes to augment microsurgical wet labs.
The Eyesi Surgical is a virtual reality (VR) simulator for eye surgery with both cataract and vitreoretinal interfaces. Due to generous grant funding from the Bruce and Wendy Hadden Foundation and the Royal Australian and New Zealand College of Ophthalmologists, and infrastructure support from the University of Auckland, a $500,000 specialised VR unit was established in the Department of Ophthalmology at the New Zealand National Eye Centre in late 2019. The unit is incorporated within the Calvin Ring, six-microscope wet lab to provide comprehensive access to wet lab, dry lab and VR facilities for surgical training in Aotearoa. Over the last year, it has been used to train vocational ophthalmology registrars in New Zealand, including those that attended the first New Zealand National Eye Centre combined VR microsurgical wet lab skills course in February 2020 (Fig 1).
Since then, the Eyesi has been utilised by many trainees, from both the North and South Islands, to acquire cataract surgical skills. It has also been used extensively for vitreoretinal training by more senior fellows.
The Eyesi Surgical simulator
The Eyesi simulator includes a surgical microscope, a model eye in a model head, a height-adjustable (operating) table, a display monitor for instructions, live-video and feedback scores, and a twin foot-pedal system with controls identical to the operating theatre microscope (Fig 2). As various handheld instruments are introduced into the eye, these appear in the three-dimensional VR image that is viewed through the binocular microscope (Fig 3). A large, wall-mounted secondary display unit is useful for re-playing tasks for one‑to‑one feedback from a clinical supervisor as well as for group teaching.
Fig 2. The Eyesi Surgical simulator
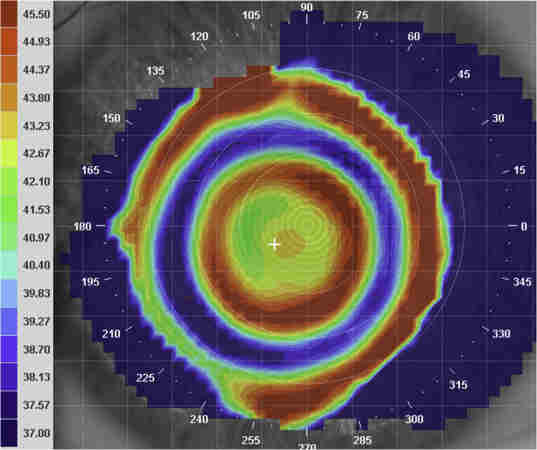
Fig 3. The surgeon views the instruments and VR procedure via the microscope, as in theatre, while supervising tutors can simultaneously view the surgeon’s technique on a large screen
The cataract modules available on the Eyesi Surgical platform are organised in stepwise levels of difficulty. The simulator provides written instructions for each task, which can be viewed via a video presentation prior to starting. The manual and bimanual dexterity tasks, anterior chamber and intracapsular navigation, as well as anti‑tremor training are useful to acquaint the new user with the simulator. The capsulorhexis task, often difficult for beginners to master efficiently, has been particularly popular among registrars. This module progresses through low, medium and high tension capsulorhexis settings of increasing difficulty.
Detailed performance analytics are conducted and quantitative feedback is automatically provided to the user immediately after each task. The task evaluation is formatted in a confidential, domain-based, quantitative manner in addition to an overall task score. For example, evaluation parameters in the capsulorhexis task include target achievements (eg. scoring each of: roundness, distance of rhexis centre to pupil centre, deviation from a 2.5mm radius, maximum radial extension and local irregularity of the rhexis), tissue treatment (eg. touching the corneal endothelium), maintenance of the red reflex, efficiency and instrument handling. These performance parameters can be used for self-comparison and progress assessment as well as anonymous comparison with other users.
Previous studies on the utility of the Eyesi Surgical simulator in an ophthalmology training curriculum have proven construct validity for several modules in the cataract platform1–4. Studies have found that when trainees participate in Eyesi Surgical training, they acquire surgical proficiency earlier in training5, while operating room performance improves up to 38%5,6 and there is an impressive reduction of intraoperative complication rates by between 33% to 53%5,7,8. Results of a study comparing 30 trainees in their first and third-year of training suggests that Eyesi performance may identify early trainees that require supplemental training9 allowing for early intervention to rectify any weaknesses.
The opportunity for training through repetition, trialling new or infrequently used techniques as well as performing challenging tasks in a risk-free environment are also beneficial to all Eyesi users. It is well known that some steps of cataract surgery are more difficult to learn than others9. Specifically, due to the use of local anaesthetic, in-depth teaching in theatre about a procedure can be challenging for trainers, trainees and may be disconcerting for patients who are typically awake during surgery. The surgical simulator overcomes this barrier by creating the opportunity for repetition of steps of increasing complexity that cannot be repeated or taught in detail while in theatre.
Who is currently using VR surgical skills training?
The virtual reality set-up at the University of Auckland has already been utilised by nearly half of the country’s vocational ophthalmology registrars, with some booking the simulator for several, three to four-hour sessions. New users can pre-arrange for a session tutor, either a credentialed consultant or senior surgical fellow, to provide one-on-one direct feedback and training. Tutors so far have included Drs Michael Merriman, Sue Ormonde, Kenneth Chan, Charles McGhee, Rachael Niederer, Mo Ziaei and Alexandra Crawford. University research staff, Dr Jie Zhang and Joyce Mathan, also provide technical support and initial orientation and are on site to navigate software and troubleshoot.
As knowledge about the availability and utility of the Eyesi system has spread, a number of consultants and fellows wishing to experiment with newer techniques or perform uncommon tasks – such as dealing with capsule rupture and vitreous loss, zonular weakness or hyper-mature cataracts - have begun to use the device. The RANZCO New Zealand branch has even provided seed funding, so that many consultants can access the device for a four-hour session free of charge.
Regular microsurgical courses, including wet lab and VR training, will re-commence in November with the Covid-19 lockdown returning to level 1. While one of the authors of this article, Dr Corina Chilibeck, is specifically pursuing a variety of research opportunities on the device10.
How near is VR training to reality?
The set-up of the physical components (the eyepiece, operating table and food pedals) was intuitive for most trainees. Generally New Zealand registrars were impressed by the three-dimensional augmented reality view of the operated eye and the life-like response of the eye to handling (or mishandling). Trainees also found the immediate domain-based feedback invaluable for improving independent practice as well as during teaching sessions with a clinical tutor. Those early in their training also appreciated the opportunity to learn and practise basic techniques, such as capsulorhexis and divide and conquer phacoemulsification, under the guidance of senior clinical tutors. However, once they were competently using the instrument on their own, the system’s guiding features, such as the depth display of the surgical instrument in the anterior chamber, were found to be very useful. The scoring of key performance parameters was felt to be accurate and included specific assessment of elements that surgeons may find difficult to self-assess.
Trainees with more surgical experience valued the ability to experiment with different techniques in a virtual environment with no real-life consequences. They also appreciated the advanced course challenges that kept them on the edge of their seats, including high capsular tension, capsular tears, weak zonules, the Argentinian flag event and dense or milky cataracts. Comparing the overall task score out of 100 was a motivator, creating a friendly, competitive undercurrent among registrars and clinical tutors, with some trainees ultimately obtaining an overall score of 100 for some difficult tasks! Supervising surgeons with the Auckland District Health Board have already identified a noticeable difference in the surgical skill of junior trainees that have spent time on the simulator.
As expected for a simulator, the Eyesi does not completely replicate real life. For example, some New Zealand trainees noted that instrument handling required more finger strength, the ‘normal tension’ capsule felt a little more elastic and the crystalline lens felt more juvenile making it stickier and more difficult to crack. However, most trainees agreed that the realistic environment and risk-free, repetitive, progressively more difficult, task structure provided by Eyesi far outweighed any minor limitations. Several registrars have already returned for more advanced sessions, taking up to 30 hours, confirming its effectiveness as a training tool.
Accessing the NZ National Eye Centre surgical simulator
The Eyesi Surgical suite can be booked for individual use with a supervising tutor via Maree McInerney (m.mcinerney@auckland.ac.nz). Training on the Eyesi Surgical simulator is also featured as part of the New Zealand National Eye Centre Microsurgical Skills Course, which is suited to vocational and non-vocational ophthalmology registrars, and recommenced in November 2020, following the move to Covid-19 Alert Level 1.
References
- Spiteri AV, Aggarwal R, Kersey TL, Sira M, Benjamin L, Darzi AW et al. Development of a VR training curriculum for phacoemulsification surgery. Eye 2014; 28: 78–84.
- Selvander M, Asman P. Cataract surgeons outperform medical students in Eyesi VR cataract surgery: evidence for construct validity. Acta Ophthalmol 2013; 91: 469–74.
- Selvander M, Åsman P. VR cataract surgery training: learning curves and concurrent validity. Acta Ophthalmol 2012; 90: 412–17.
- Jacobsen MF, Konge L, Bach-Holm D, la Cour M, Holm L, Højgaard-Olsen K et al. Correlation of VR performance with real-life cataract surgery performance. J Cataract Refract Surg 2019; 45: 1246–51.
- Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg 2011; 37: 1756–61.
- Thomsen ASS, Bach-Holm D, Kjærbo H, Højgaard-Olsen K, Subhi Y, Saleh GM et al. Operating room performance improves after proficiency-based VR cataract surgery training. Ophthalmology 2017; 124: 524–31.
- Ferris JD, Donachie PH, Johnston RL, Barnes B, Olaitan M, Sparrow JM. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 6. The impact of Eyesi VR training on complications rates of cataract surgery performed by first and second year trainees. Br J Ophthalmol 2019. doi:10.1136/bjophthalmol-2018-313817.
- Staropoli PC, Gregori NZ, Junk AK, Galor A, Goldhardt R, Goldhagen BE et al. Surgical simulation training reduces intraoperative cataract surgery complications among residents. Simul Healthc 2018; 13: 11–15.
- Taravella MJ, Davidson R, Erlanger M, Guiton G, Gregory D. Characterizing the learning curve in phacoemulsification. J Cataract Refract Surg 2011; 37: 1069–75.
- Chilibeck CM, McGhee CNJ. Editorial. VR surgical simulators in ophthalmology: Are we nearly there? Clin Exp Ophthalmol. 2020;48(6):727-729.
Dr Corina Chilibeck is an anterior segment clinical research fellow. Her doctoral studies are based on aspects of cataract surgery, surgical risk and surgical training, including the Eyesi Surgical simulator.
Joyce Mathan is an optometrist and doctoral candidate, whose PhD research focused on keratoconus and Down syndrome.
Dr Jie Zhang is a senior research fellow and translational vision scientist whose research focuses primarily on corneal regeneration and endothelial disease.
All are based in the Department of Ophthalmology, headed by Professor Charles McGhee, at the University of Auckland.