When makeup gets in the way
In 2014 I was in my final year overseas preceptorship, shadowing a middle-aged male optometrist. The patient was a lady in her forties. He was on the slit lamp. “Hmm… do you see that?” he asked me. “Madarosis. Could be an autoimmune cause. We need to send her for a blood workup. What tests would you ask for?” The lady looked at me awkwardly. She and I knew that this was not the issue. My tentative diagnosis: lash extensions in their third or fourth week, when shedding is bound to occur!
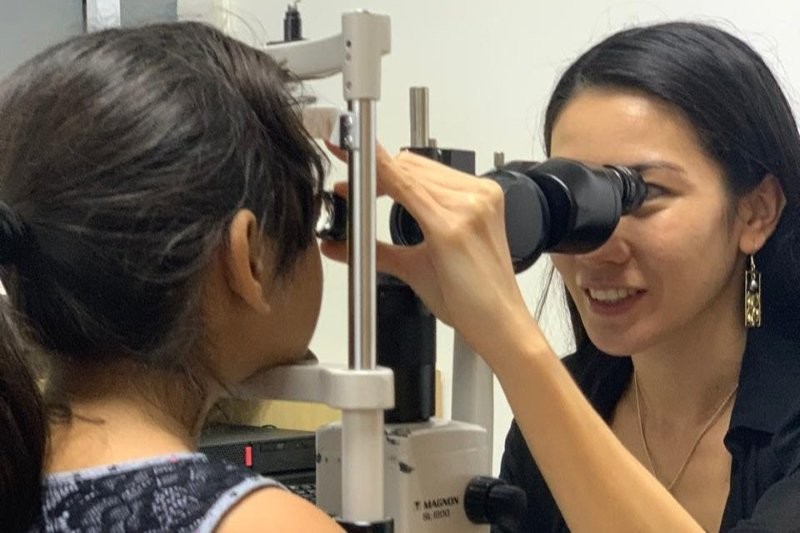
Throughout my years of practice, I have noticed the increasingly common use of beauty products and services among women of all ages and there is a disparity between what they feel comfortable disclosing to a male optometrist and a female one. Here, I’ve tried to bridge that gap, using some real cases together with insights from oculoplastic surgeon Dr Paul Rosser, who was recently made the first honorary member of the New Zealand Society of Cosmetic Medicine, and beauty therapist and lash lift trainer Maz Hussein.
The trouble with eyelashes
False eyelashes
I once had a 21-year-old present to clinic complaining of a painful eye with fluctuating vision. She had a corneal abrasion and, looking through her file, I noticed this had happened more than once. After asking, I discovered she frequently wore false (strip) lashes. Depending on lash material, density, length and curvature, strip lashes and lash extensions can have an abrasive action on every blink. It’s important that as clinicians we are aware of this, as recurrent abrasions can not only impact refraction and patient symptoms, but also increase the risk of opportunistic infections and sequelae of recurrent corneal erosion.
Another anecdotal finding that correlates with women with dense lash extensions (myself included!) is incomplete blink and/or nocturnal lagophthalmos. I asked my colleague to monitor my eyes and we found that my nocturnal lagophthalmos, secondary to lash extensions, made my eyes feel more gritty, consequently increasing my eye rubbing and the grade of my superior tarsal papillae. I would recommend monitoring risk of allergic conjunctivitis in lash-extension wearers, especially because there is a large overlap between girls who wear them and contact-lens wearers. Fluorescein staining and lid eversion is always a good idea, especially for your more heavily made-up patients.

Thermal burn secondary to cyanoacrylate-based glue used to apply eyelash extensions. Credit: Nardeosingh and SeeWah Tung³
The active ingredient in the adhesive used in lash extension application is ethyl cyanoacrylate, which sets exothermically as it comes into contact with moisture. This rise in temperature can cause a thermal burn. This is an important differential diagnosis to keep in mind with erythematous and oedematous lids post-lash-extension application. Most important, however, is contact dermatitis. As Maz Hussein points out, “One of the biggest barriers is that clients don’t always accurately disclose the medications they are on. For example, it’s becoming increasingly common for women to use retinoids, as they are no longer just used as acne medication but are recognised for their anti-ageing properties. Clients forget to mention they are using this topically on their face and it can increase their risk of dermatitis and other skin reactions.”
False lashes aside, sometimes you might notice some patients have long but aberrant lashes and surprisingly low intraocular pressures. Does this sound familiar? While off-label use of prostaglandin analogues is common, Dr Rosser points out that this medication “can produce unruly lashes as well as a change in eyelid skin colour and iris pigmentation. Patients at times request glaucoma drops to apply to their lashes, but it is better to use one of the specially produced products such as LiLash, which have applicators allowing the drug to be more accurately applied.”
Cosmetic interventions are not always vanity related. I had a 21-year-old female patient with entropion that was continually causing corneal abrasions, as well as unstable tear film from compensatory blink patterns. We experimented with sending her to get a ‘lash lift’ for her lower lash margin. This treated her entropion without the invasiveness or negative cosmetic impact of alternative modes of therapy such as Botox, cautery or lid tape.
Messing with eyelids
Some of you may have heard of the ‘fox eye’ trend, where celebrities such as Bella Hadid and Kendall Jenner have a pulled-back effect to their eyes. Though many women simply use makeup to achieve a partial fox-eye effect, some go a step further, attempting to gain it surgically through a combination of blepharoplasty and canthoplasty. This trend has lowered the age range of patients having these procedures performed. Typically, side effects of any significance are rare with upper lid surgery, owing to the richness of blood supply in the region, says Dr Rosser. However, with the younger demographic, sometimes too much skin is removed and this can reduce eyelid closure and cause subsequent punctate staining. Fat debulking from these procedures can also produce a hollowing of the eyelids and create a premature ageing effect, so an alternative and more affordable way of achieving this look is through the use of Botox injections.
Patients may present with an acute unilateral ptosis. We would expect most patients who have had Botox injections to disclose that fact, but I had one patient who said nothing to the male optometrist she initially saw. But when he passed her to me, she told me. As Dr Rosser says, “A drooping of the upper lid is seen at times with patients undergoing treatment to the periorbital area.” This is because the botulinum toxin can migrate to and paralyse the levator palpebrae.
Right eye ptosis following Botox injections. Credit: Akkaya et al⁴
A very common treatment for this is the off-label use of a topical alpha-2 agonist such as apraclonidine, which can help reduce botulinum-toxin-induced ptosis, says Dr Rosser. “But this usually takes a few weeks to fully resolve.” Apraclonidine stimulates the contraction of Muller’s muscle to raise the upper eyelid 1-3mm. Clinical guidelines and optimal dosing of apraclonidine in the temporary relief of botulinum-toxin-induced ptosis are still yet to be established¹. In the case of my patient, the nurse who had administered the injections had sourced the apraclonidine for her, so she was advised to just use the drops as needed. The patient over-used the drops (at first using them bid-qid, before increasing to six times a day), and noticed an improvement after the first week of use, followed by a worsening over the second, which is what brought her in to see us. In this case, the causative issue was a follicular reaction as part of an acute allergic response triggered by the topical use of apraclonidine. I regulated her use of the apraclonidine and advised compliant use of a topical corticosteroid, cool compresses and artificial tears. After a week, the patient’s second round of ptosis had resolved.
This was a good case reminder of botulinum toxin as a differential diagnosis for the cause of acute ptosis and to evert the eyelid. Dr Rosser also advises that, “In some cases there may be reduced lid closure from injections to the ‘crow’s feet’ lines. This is a well-known complication due to effects on the orbicularis muscles,” which serves to reinforce the fact that fluorescein testing is essential.
Lower-lid blepharoplasty is becoming an increasingly common cosmetic therapy for women aged 50-plus. Although little research has been conducted on postoperative effects of lower blepharoplasty in that age group, a common side effect is persistent diplopia lasting more than a week (most frequently involving the inferior oblique muscle) during recovery from surgery². Therefore, lid surgery is an important differential to keep in mind with new-onset diplopia. In most cases it will resolve completely without further intervention.
In conclusion
I feel the age-old saying rings true: ‘beauty is pain… or at least it can be!’ It is our role as clinicians to be cognisant of the potential side effects that can come with these cosmetic services to better look after, manage and advise our patients. There will always be more to learn, since the beauty industry is ever changing, but I hope this article can serve as a good starting point. I would like to add that these cosmetic processes can be beneficial! After managing my blink pattern, lash density and switching to a latex-free, formaldehyde-free adhesive, false (strip) lashes are helping my tear film do better than ever; they’ve even improved the meibomian gland dysfunction I used to have from long-term mascara use!
References
- https://www.aaopt.org/docs/knowledge-base/michelle-crist.pdf?sfvrsn=2d755592_0
- https://www.reviewofoptometry.com/news/article/blepharoplastyinduced-diplopia-more-common-than-previously-thought
- https://www.thepmfajournal.com/features/features/post/thermal-injury-and-false-eyelashes
- https://www.thepmfajournal.com/features/features/post/thermal-injury-and-false-eyelashes

Australian-based optometrist Layal Naji is a lecturer of optometry at the University of Canberra and co-founder of the outreach optometry clinic at the Asylum Seekers Centre in Newtown, Sydney.