YAG laser for optoms proposed
Following a successful pilot study, the Optometrists and Dispensing Opticians Board (ODOB) has released a consultation document for a new specialist optometrist scope of practice to allow hospital-based optometrists to perform ophthalmic laser surgery.
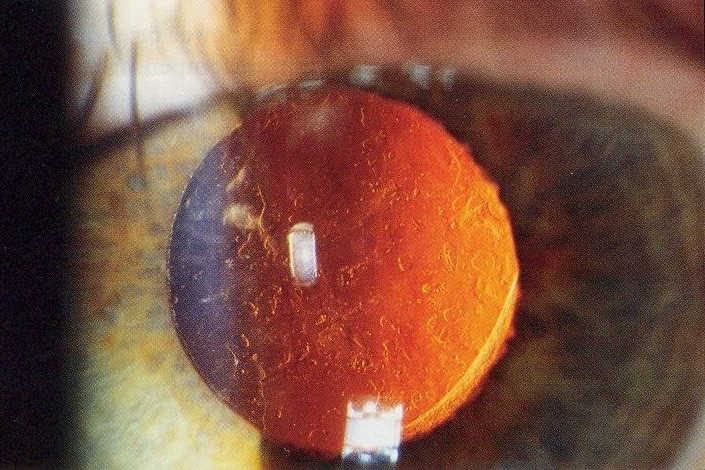
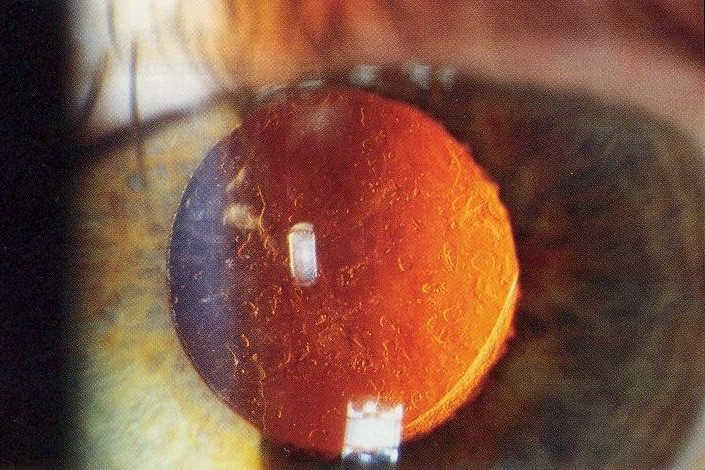
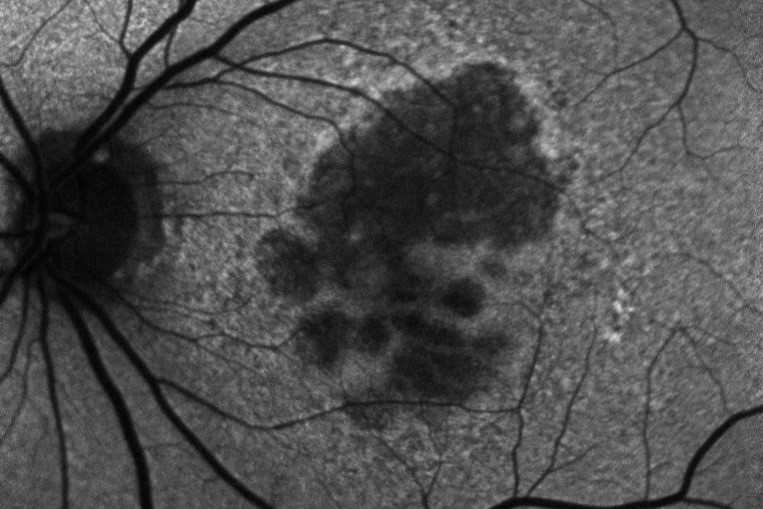
Specifically, the specialist scope of practice relates to the use of neodymium-doped yttrium aluminium garnet (Nd: YAG) for laser capsulotomy and peripheral iridotomy. YAG laser capsulotomy is a relatively non-invasive procedure most often used to treat posterior capsular opacification following cataract surgery, while peripheral iridotomy creates a tiny hole in the iris to prevent acute angle closure glaucoma.
In its strategic plan, one of the board’s goals is to analyse and identify workforce demand and public need, said ODOB chair Jayesh Chouhan, and YAG laser was identified by both the district health boards (DHBs) and the board as one such need. “By freeing ophthalmologists for more complicated procedures this would have the effect of reducing overall waiting times for all ophthalmic treatments, improving treatment efficiency and therefore reducing unnecessary impairment of vision,” wrote the ODOB in the consultation document.

ODOB chair Jayesh Chouhan
Under the Health Practitioners Competence Assurance Act 2003, optometrists can prescribe the use of any ophthalmic appliance for the correction of sight defects, but the YAG laser scope would require an additional restricted activity to allow optometrists to perform surgical procedures “below the mucous membrane or surface of the skin”. Thus the ODOB approached Auckland DHB to arrange a pilot study to test the parameters and protocols for training to allow an optometrist to give YAG laser in a safe and effective manner. The protocols were developed from similar documentation developed for nurses in New Zealand and for optometrists in the US and UK, where specially trained optometrists have been providing YAG laser for many years. Key to the protocols is the need for the training optometrist to have worked in a DHB for at least three years; to have at least 400 hours in the relevant clinic; and to have a registered ophthalmologist to train and supervise them. “We kept in mind what optometrists know already and what they may need to know in doing this, so for example, understanding laser,” said Chouhan.
To ensure objectivity, the pilot was arranged with the support of Dr Sarah Welch, clinical director of the Auckland District Health Board Ophthalmology Service, and two supervising Auckland-based consultant ophthalmologists, cataract surgery specialist Dr Andrew Riley and glaucoma specialist Dr Hussain Patel, who oversaw Greenlane specialist optometrist Richard Johnson. The pilot kicked off in March last year but was delayed several times due to Covid, with all elective surgery postponed during certain lockdown levels.

Dr Sarah Welch, clinical director of the Auckland DHB Ophthalmology Service
Dr Patel, Dr Riley and Johnson were unable to comment until after the consultation period, however Chouhan confirmed the pilot was successful. “From the feedback, including the supervising ophthalmologists as well as the outcomes of the pilot, this is a really robust, safe and well-structured process, so I feel quite positive that this will be successful in implementation,” he said.
Dr Welch said, “We like everyone to work at the top of their game, at the top of their scope and we have some optometrists who are extremely experienced and, as a good manager, you have to support your staff to grow and develop. The key thing is the optometrist has ongoing supervision and support from the associated ophthalmologist, ensuring ongoing safety.
Both Dr Welch and Chouhan agreed this new specialist scope will only appeal to a very small number of optometrists. “At ADHB we really try to use our nurses and our allied staff as much as possible to try and maximise everyone’s skills and enable us to see as many people as possible because we’re always bursting at the seams,” said Dr Welch. “So this will enable us to see a few more people which is always a good thing… patients will still be given the same standard of care and be under an ophthalmologist - it’s just another way of increasing our overall eye workforce.”
The consultation is open to everyone, with submissions required before 22 December: https://www.odob.health.nz/wp-content/uploads/2021/04/C1-ODOB-Laser-Consulation-Paper.pdf