You too can laser!
Northland nurse practitioner Fiona Bamforth is the first ophthalmic nurse in New Zealand to perform YAG laser capsulotomy and peripheral iridotomy and is calling on more nurses to take the plunge and do laser.
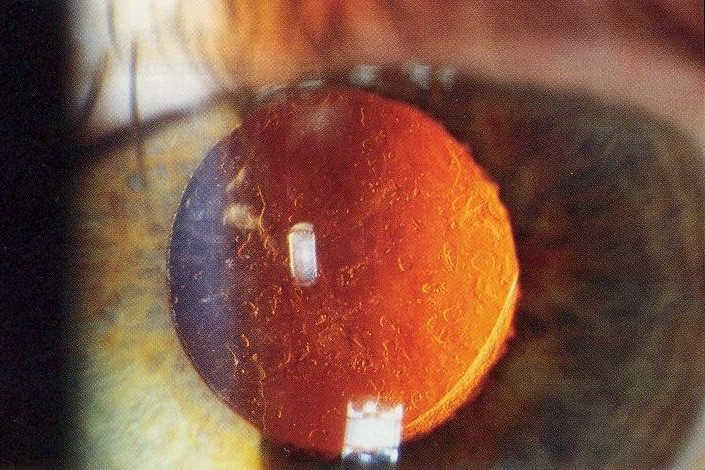
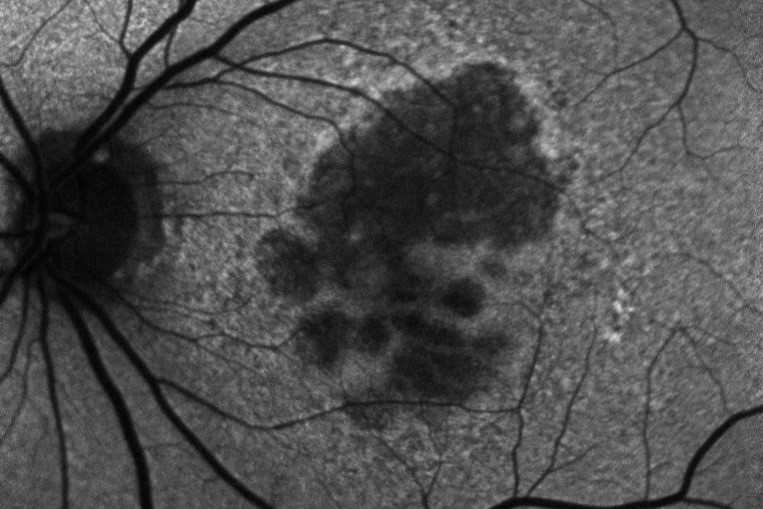
Neodymium-doped yttrium aluminium garnet (Nd:YAG) laser capsulotomy is a relatively non-invasive procedure that is used to treat posterior capsular opacification, a common complication of cataract surgery, while peripheral iridotomy (PI) is used to treat narrow angles, narrow-angle glaucoma or acute angle closure glaucoma. Both are commonly performed by ophthalmologists, though in the UK’s public system they are now primarily undertaken by nurses and other allied health staff.
In her presentation at the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) NZ Branch meeting, Bamforth said she decided to do YAG laser after being encouraged by her ophthalmologist colleagues because of treatment delays and disruptions for her patients. “Since I’ve become a nurse practitioner, I’ve been really independent with managing my patients, so having to interrupt doctors’ clinics to ask them to laser my patients felt like the whole continuity of care was dropping away.”
Bamforth, who’s been an ophthalmic nurse since 1993, was also the first nurse in New Zealand to perform sub-Tenon’s block, the most common form of orbital regional anaesthesia, and is an experienced intravitreal injector. To provide YAG laser, she undertook a laser safety course, had a comprehensive introduction to laser technology by a medical rep and was trained by two ophthalmologists and one registrar before completing 20 supervised YAG laser procedures and taking over the practice herself. Since July last year she’s performed 148 procedures – about 30% of the clinic’s lasers – with only very minor (and common) complications, and is now keen to expand her laser experience into photo-thermal iridotomy, focal laser for diabetics and, because of her glaucoma patients, selective laser trabeculoplasty, she said. The support of your colleagues and knowing how to work a slit lamp and hold a contact lens on the eye are all you need to do laser, she said. “It’s just about a change of roles, a different way of thinking. There are a lot more things that we do as nurses that are more technical.”
Dr Sarah Welch, clinical director of the Northern Regional Ophthalmology Service, also supports ophthalmic staff taking on expanded roles to support better patient care in New Zealand.
“The reason the Northern Regional Ophthalmology Service was set up was to try and reduce inequity across the region. We’re doing everything to work to try and support people in areas of need and that means developing expanded practices and new skills to safely treat our patients,” she said.
In her previous role as clinical director for Auckland District Health Board (ADHB), Dr Welch said she had been a strong supporter of increasing the ophthalmic team’s auxiliary workforce and was proud of the number of nurse specialists and nurse practitioners ADHB now had. “Our department couldn’t function without them. The transition to nurse injectors for Avastin has been transformational in how we’ve managed the huge increase in patient visits and treatments. I understand departments have different needs in different areas but where there is need, I will always support someone who has been properly trained to expand their practice and who can deliver care in a safe way.”