Eye Surgery Associate’s winter’s tale
Starring Tauranga-based ophthalmologist Dr Cheefoong Chong, heading a stellar supporting cast of Drs Hussain Patel, Monika Pradhan, Yi Wei Goh and Tracey Wong, Eye Surgery Associates presented another highly anticipated sequel in its annual seminar series.
Dr Chong’s subspecialties are paediatric ophthalmology, strabismus and retinoblastoma, plus cataract and refractive surgery. He is also the lead ophthalmologist in the National Retinoblastoma Service. His first topic of the evening focused on the challenges and advances in paediatric ocular oncology. The history of treatment, from enucleation in the early 19th century to intravitreal and intracameral chemotherapy in the 21st century, was both a sobering start to the night and a reason to celebrate the progress of science. According to Dr Chong, there are a lot of new treatment modalities in the toolkit including, “keeping eyes in children’s heads more than 80% of the time”, providing the cancer is caught early enough. One such retinoblastoma treatment, intra-arterial chemotherapy, was performed in New Zealand for the first time late last year.
Seeing red for retinoblastoma screening
Retinoblastoma is both the most common and most serious cancer in children. It is recognised mainly by leukocoria, strabismus and/or proptosis (always a bad prognostic sign). A family history of a parent having had an eye enucleated is also a red flag. Leukocoria, or lack of a red reflex, is present in 80% of cases and is currently the main screening tool used. The big take-home from this talk was that red reflex is not an effective way to screen for eye tumours. Firstly, in an undilated pupil only 2% of the retina is seen at any time, making it a good screening tool for cataracts but terrible for spotting cancers, which require the fundus to be viewed directly. An audible gasp was heard around the roomful of optometrists when Dr Chong went on to say the second reason was because the red reflex is not always red! It is only red in Caucasians! An Asian child will have a yellow reflex, an African a blue colour and in a Māori or Pacific Islander it looks dull or a bit bluish. For this reason, the red reflex is now called the fundal reflex. Cancer, however, still needs the earliest possible diagnosis, so any child with a suspicious fundal reflex or strabismus needs a dilated fundus examination and cycloplegic refraction.

Alice Ku, Jennifer Lu, Kathreena Lim and Anh-Dao Le
Retinoblastoma is thought to occur in 1 in 17,000 live births in New Zealand and most of those affected have no known family history of an eye enucleation at an early age, or do not think to mention it. Questioned on why parents with a family history of ocular tumour do not get genetic testing in New Zealand, Dr Chong replied that it’s because of a lack of public education and awareness.
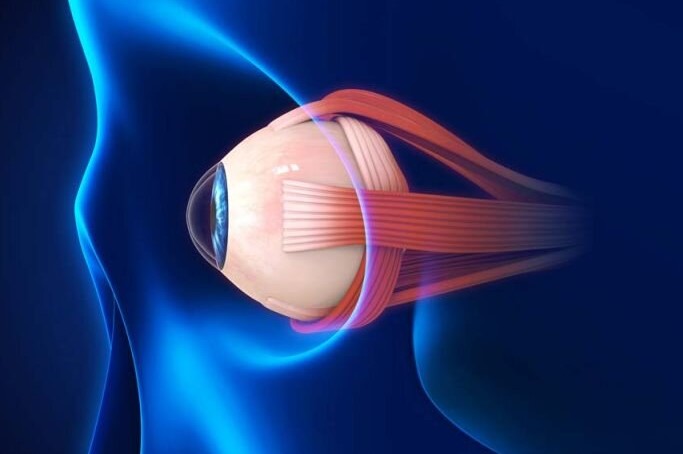
Challenging palsy mimics
Dr Chong’s second presentation was on superior oblique palsy (SOP) and its challenging mimics. This is a common palsy, particularly of traumatic origin. A large survey of US ophthalmologists, however, found 50% of SOP diagnoses were incorrect due its many mimics. The symptoms to look for include binocular oblique diplopia (worse in the contralateral gaze and ipsilateral head tilt), with compensatory head posture featuring ipsilateral face turn and contralateral head tilt, and symptomatic torsion. Patients may also have a spread of comitance with vertical diplopia. This was a lot to chew on before the main course even arrived!
To simplify diagnosis, Dr Chong suggested asking the patient to look at a horizontal surface, such as the edge of a desk, then ask if they see two lines and if one is tilted relative to the other. These symptoms appear to get worse when the head is tilted towards the worse eye. He also advised looking at fundus photos or OCT to compare the fundus orientation. Is the macula in the same horizontal line from the disc in both eyes? The torsion of one fundus relative to the other is an important diagnostic test for acquired vertical deviation, he said. A skew deviation is defined as any acquired vertical strabismus resulting from an imbalance in vestibular inputs to the ocular motor system. The pathological ocular tilt reaction is the triad of skew deviation plus binocular conjugate torsion (ocular roll to counter roll) and head tilt. The big take-home message was to look at the fundus. This could not just be life-changing but life-saving!
Ergonomics for ECPs
With the assistance of technology, it was easy to be persuaded that Dr Monika Pradhan was beaming in from a lounger on her favourite Pacific island beach resort to tease us winter-bound attendees. The reality was she was just emerging from isolation and – taking note of Dr Malcolm McKellar’s excellent July 2023 Chalkeyes article on how to be a superspreader of knowledge rather than bugs – was presenting via Zoom. Her topic of ergonomics to protect your back was well received, even by those of us who are vertically challenged.
An Australian study showed 82% of the country’s optometrists had neck, back, shoulder and arm problems, while a survey of American ophthalmologists showed nearly 52% had neck, back or upper extremity problems, with more time spent operating equating to more pain experienced. Risk factors include repetitive tasks requiring fine motor control, especially under stressful circumstances, as well as a lack of back, wrist and upper-arm support. Simple postural alterations, such as reclining the patient during retinoscopy and refraction, may reduce the time spent in ‘non-neutral’ postures, reducing the likelihood of musculoskeletal injuries. I have some doubts about keeping the reclining patient fixated on a distant target with eyelids open long enough to do a ret, however, let alone a subjective refraction. ‘Please keep your eyes wide open while I recline the chair and dim the lights’ doesn’t sound very wholesome either!

Frank Snell, Carolyn Campbell and Angela Garner
Perhaps a safer alternative is practitioner support, particularly for raised arms when at the slit lamp or operating. It’s also a good idea to avoid resting your arms and wrists on hard surfaces, she said, as this can lead to cubital tunnel syndrome of the elbows or carpel tunnel syndrome of the wrists. Dr Pradhan recommended wearing comfortable clothes and shoes when at the slit lamp; using soft gel elbow and wrist rests; and, when sitting directly in front of the patient, asking them to bring their chair forward, rather than leaning forward or hunching over the slit lamp. Raising the patient’s chair and/or lowering the practitioner’s chair is important for maintaining a comfortable posture, and don’t cradle your phone between your ear and shoulder.
These things also apply to computer workstations and operating theatres, where adjusting table height and angle of eyepieces is necessary. Having a chair with arm rests is important, particularly for lengthy surgeries. I wonder how much the hot-desking trend has contributed to some of these problems – not having your own setup to accommodate your specific needs must surely be an exacerbating factor.
The final word from Dr Pradhan before she melted back into her tropical island background was to take microbreaks and do some stretches. Self-care is important for health professionals, she stressed.
GA – an update
Dr Tracey Wong updated us with the exciting progress being made in treating geographic atrophy (GA), with clinical trials involving the complement system (part of the immune system). In particular, the one- and two-year results of the Oaks and Derby studies on pegcetacoplan, encompassing over 1,200 patients from 232 sites with the drug injected intravitreally once per month or alternate months and compared with a sham injection group on the same regime. The studies showed a slowing in the growth of GA lesions and a reduction in the loss of retinal pigment epithelium and photoreceptor cells, with increased effect over time. This was particularly evident in the non-subfoveal cells. Overall, there was a difference of five letters in vision between treatment and non-treatment groups.

Colin Li and Wen Li Keng
An interesting observation was that the greatest benefit appeared to be for extra-foveal lesions, with a significant change in quality-of-life measures. The reduction of the extra-foveal ring scotoma, while not producing a huge measurable improvement in acuity on the distance chart, would no doubt be saving functional ability in terms of reading, which would account for the improvement in quality of life. Our excitement, however, was tempered by the finding that this treatment appears to increase the risk of wet AMD onset; the reasons for this are unknown at present. There will be more information available from the Gale study, which is extending the data to three years.
Dr Wong said this treatment may be available in Australia from early next year, with the caveat that it’s likely to be very expensive. There is a similar drug in the pipeline, so we are in for an interesting couple of years, tempered of course by the anxiety of any new treatment involving the macula.
Juggling the CPAC score
The evening continued with a small juggling act featuring Dr Yi Wei Goh and her treatment of the cataract surgery waiting list and the national CPAC score. Visual acuity is not sufficient information to indicate need, she said, but by adding more information, optometrists can help ascertain urgency, which benefits both patient and surgeon. Snellen acuity is not the only important statistic, since the type of cataract can impact contrast sensitivity, glare disability and glare recovery, particularly with night driving. These additional measures may indicate the reduced quality of vision.
Ultimately, the risks-versus-benefits must include other patient factors such as occupation, need to drive, caregiving for dependents and motivation for surgery, she said. Diabetes and glaucoma are obvious elevators, but additional medical information – such as tolerance for local or general anaesthetic, tight orbit, whether the patient can lie flat, or is on alpha-blocker treatment – will help determine whether they can go onto a registrar list or need more specialised care. Other ocular factors such as dry eye, blepharitis and pterygium should be noted and, where possible, treated before cataract surgery. Dr Goh stressed the need to include information on dementia so the patient knows to bring their enduring power of attorney with them to sign consent forms, otherwise the appointment will be wasted.
The final act
The evening returned to the topic of self-care with Dr Hussain Patel’s entertaining, enlightening and self-effacing presentation on managing the unhappy patient. It was a topic we could all learn from, not only for our own and our team’s health, but also to give the heads-up to the ophthalmologist when referring that ‘challenging’ patient. Dr Patel stressed it’s a team effort and optometrists know their patients best, particularly if they have a long history with them and managing their expectations. He suggested having a ‘game plan’ for the whole team when confronted with an unhappy or angry patient, to provide the best opportunity to correct the situation before it escalates. There was a consensus in the room that these situations are arising more often, with people generally under a lot of pressure and on shorter fuses.
Dr Hussain’s last message was that you need to have a back door built into your practice! It was sound advice to draw the curtain on a very successful evening amid generous applause and laughter.
Pictures by Naomi Meltzer and Maryanne Dransfield

Naomi Meltzer is an experienced optometrist who now runs an independent practice in Auckland specialising in low-vision consultancy. She is a regular contributor to NZ Optics.