Mitigating ectasia risk
Corneal ectasia is, realistically, the worst complication following corneal refractive surgery and a major cause of litigation, medicolegal complaints and unhappy patients following otherwise routine laser eye surgery.
Ectasia occurs because the laser procedure has weakened the cornea to the point where it cannot adequately resist the stress induced by normal intraocular pressure. The cornea becomes progressively distorted and thinned in a process very similar to progressive keratoconus, resulting in poor-quality vision. While collagen crosslinking is usually successful in halting keratoconus progression, glasses or rigid contact lenses may be required to obtain satisfactory vision.
The risk factors for the development of ectasia have been known for many years and include abnormal preoperative corneal topography or tomography, younger age (<34 years), family history of keratoconus, high myopia (>8 diopters), reduced preoperative corneal thickness and lower postoperative corneal residual stromal tissue.
Clandestine keratoconus
Prior to the development of the Orbscan and the Oculus Pentacam, placido-based topography devices were used to assess corneal shape and detect keratoconus in laser candidates. Topographic devices only assess the anterior corneal surface but cannot assess global pachymetry and posterior corneal changes. They can detect keratoconus in most cases, but because very early keratoconus may only produce changes on the posterior corneal surface, corneal topography may fail to diagnose it in a refractive surgery candidate. Such a candidate is almost certain to develop post-surgery ectasia and many early ectasia cases were likely to have had early undiagnosed keratoconus.
With the development of the Oculus Pentacam and other similar tomographic devices, it was hoped ectasia would become a thing of the past. Because such devices can assess global corneal pachymetry and posterior corneal shape, it was assumed that finding areas of subtle posterior corneal elevation or localised thinning would enable detection of very early or ‘forme fruste’ keratoconus and hence avoid performing laser refractive surgery on at-risk individuals.
Unfortunately, ectasia continues to be reported following uneventful surgery in apparently completely normal eyes. The remarkable thing is that these cases had normal preoperative corneal tomography and no pre-existing ectasia risk factors. A number of such cases had small incision lenticule extraction (SMILE) surgery. SMILE was thought to have a lower risk of ectasia because the flapless procedure purportedly has less effect on corneal stiffness than a similar correction using LASIK.
So why should corneal tomography not absolutely allow detection of ectasia risk? Current thoughts on the causation of keratoconus may help sort out the ectasia conundrum. Several things can help us think about this.
Firstly, the ‘two-hit’ hypothesis suggests both a genetic predisposition (the first hit) and an environmental factor such as eye rubbing (the second hit) may be required to develop keratoconus. Similarly, ectasia may develop in someone with a genetic predisposition who then has refractive surgery. The laser candidate may be unaware of a family history of keratoconus, and tomography cannot detect that!
Secondly, it is crucial to remember that detection of ectasia risk is not the same as detection of keratoconus. While detection of very early keratoconus is a relatively trivial task with modern diagnostic tools, ectasia can occur in tomographically normal corneas.
Thirdly, corneal tomography tells us about the cornea’s shape and thickness but almost nothing about mechanical properties such as its stiffness or elasticity – corneal biomechanics. Consider two corneas which appear tomographically identical but the first is significantly weaker than the second: the first belongs to a 10-year-old, the second to a 70-year-old. Research has shown that corneal stiffness approximately doubles between the ages of 20 and 100 years, presumably due to the natural corneal collagen crosslinking which occurs with age.
Instrumental collaboration
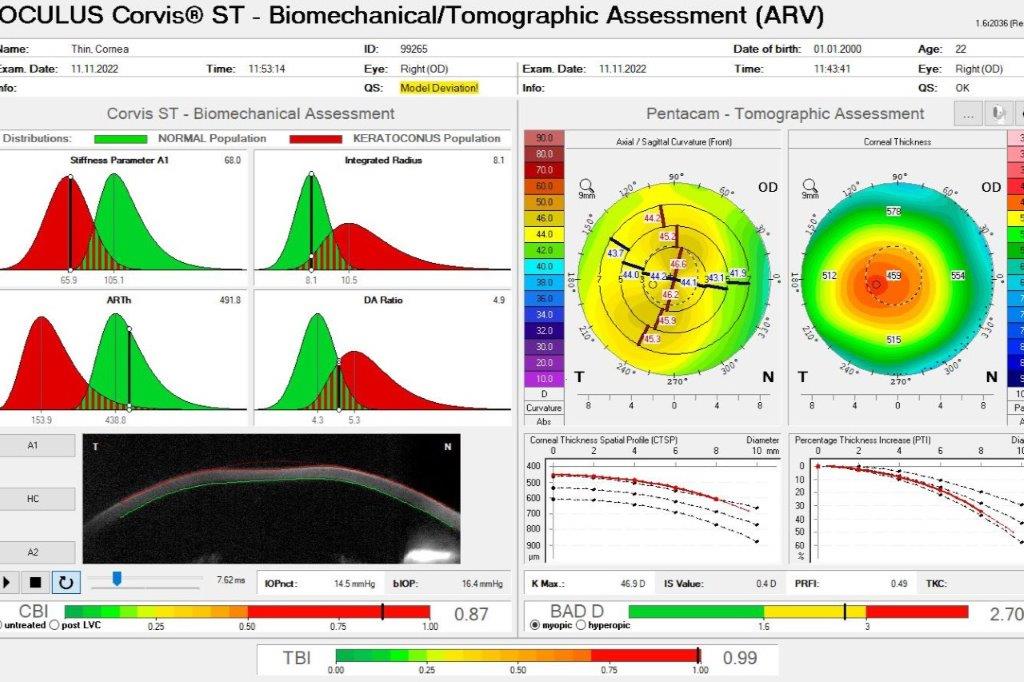
There is increasing evidence that measurement of corneal biomechanical properties, especially when combined with corneal tomography-derived data, may provide a better assessment of ectasia risk than tomography alone. Measurement of corneal biomechanics involves assessment of corneal elasticity, viscoelasticity and how the cornea responds to stress. While there are several ways to measure corneal biomechanical properties (including laser interferometry, ocular pulse elastography, Brillouin microscopy and ex-vivo mechanical testing) there are currently only two devices for routine testing in the clinic – the ORA (Ocular Response Analyser) from Reichert, and the Corvis ST (Corneal Visualisation Scheimpflug Technology) from Oculus.
Using a machine-learning methodology called Random Forests, Oculus and Brazil’s Professor Renato Ambrosio developed the Biomechanical/Tomographic Assessment, which combines tomographic data from the Pentacam and biomechanical data from the Corvis to produce the tomographic/biomechanical index, or TBI. The TBI has been shown to be an excellent detector of ectasia susceptibility and using it with an appropriate cut-off value should significantly reduce the incidence of ectasia following refractive surgery.
Additionally, at Wellington Eye Centre we use AcuSimX software, which employs the Finite Element Analysis (FEA) algorithm engineers use to predict how designs for bridges, large buildings and aircraft will react to real-world forces such as vibration, heat and fluid flow. AcuSimX takes measurements from the Pentacam, the Corvis and the measurements for the planned surgery to predict corneal strength after laser eye surgery. It requires significant computing power and typically takes just over an hour to analyse one cornea.

Dr Andrew Logan is a consultant ophthalmologist with the Wellington Eye Centre, specialising in the cornea and anterior segment and refractive surgery. He was the first surgeon to perform LASIK surgery in New Zealand in 1995, he introduced SMILE keyhole laser vision correction in 2014 and he continues to explore and introduce new technologies as they become available.