ODOB responds to ‘that RANZCO letter’
The recent letter from the Royal Australian and New Zealand College of Ophthalmologists (RANZCO), urging its New Zealand members not to train experienced hospital optometrists to do minor laser procedures, conflicts with New Zealand’s health reforms and the best interests of the public, said the Optometrists and Dispensing Opticians Board (ODOB). Responding to the RANZCO letter, the ODOB said RANZCO’s Australian head office is causing a significant trans-Tasman rift with its position against the recently created specialist optometrist scope of practice.
“We are disappointed in RANZCO’s letter to their New Zealand fellows,” said ODOB chair Kristine Hammond. “This is not only counterproductive in helping address the growing waitlists and eye healthcare inequities in the country, but it also raises serious ethical questions where there is an obligation on doctors to collaborate with colleagues to improve care.”
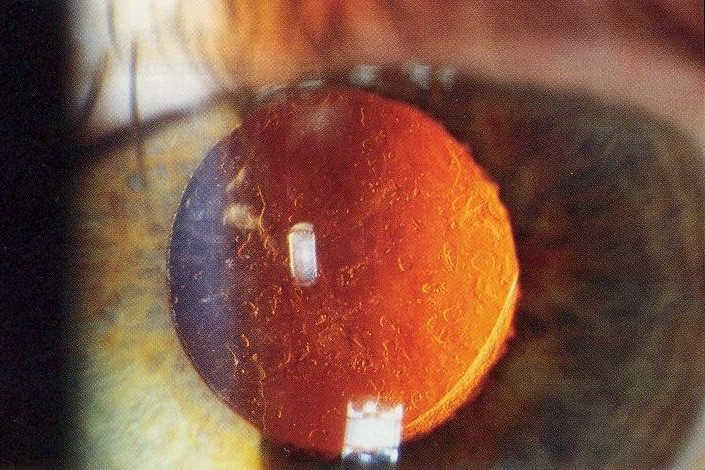
The specialist optometrist scope allows experienced public hospital-based optometrists to be trained to perform YAG laser capsulotomy to remove the film that can build up after cataract operations and laser peripheral iridotomy to create a small opening at the edge of the iris to reduce pressure in the eye. Each takes a matter of minutes, said the ODOB, and is considered low-risk surgery, yet delays to these procedures can cause unnecessary loss of vision and contribute to worsening eye health inequities. “The conditions for which these laser surgeries are indicated are diagnosed by optometrists in hospitals, who then have to refer the patient,” said Hammond. “Allowing these optometrists to perform the surgeries at the same appointment benefits both the patient and the public health system and leads to better eye health outcomes, particularly for Māori and Pasifika populations.
Optometrists have been performing these surgeries in other countries, including the UK, and the benefit to the public health sector is clear. Our New Zealand-based specialist optometrists require more rigorous training than in other countries and, while it’s still early, in New Zealand we have not seen any change in the level of surgical complications.”
Despite the support of many ophthalmologists in New Zealand – several of whom have been involved in training select hospital-based optometrists to do YAG and in the 10-month controlled pilot study designed to set detailed training guidelines – RANZCO has fought the change throughout. Though no one will say so publicly, it’s commonly believed this is due to concerns from RANZCO’s board and some senior fellows (especially in Australia, where nurses and allied health staff aren’t even allowed to give anti-VEGF injections), that this is the ‘thin end of the wedge’ that could lead to further scope advancements and thus cost ophthalmologists potential work and income. This is despite evidence to the contrary from places like the UK, where scope expansion among allied health staff is common. This has also led to a push in New Zealand to extend the ability of hospital-based optometrists to give anti-VEGF injections, like their UK counterparts, through an additional scope change – a push gaining more traction, given the current shortage of nursing staff. RANZCO, however, maintains its opposition, citing patient safety – a concern dismissed by the government when accepting the laser scope change, given the significant clinical evidence from overseas.
“We have always had a very good relationship with the New Zealand-based fellows of RANZCO and share a vision of improving eye health efficiencies and reducing health inequities,” said Hammond. “We trust that the Australian-based fellows of RANZCO won’t get in the way of the New Zealand health system finding innovative and safe ways to provide the needed eye healthcare every New Zealander deserves.”