Paediatrics research review
Low-concentration atropine eyedrops for myopia control in a multi-racial cohort of Australian children: a randomised clinical trial
Lee S S-Y PhD, Lingham G et al
Clinical and Experimental Ophthalmology 2022:50(9);1001-1012
Review: This single-centre, double-masked, parallel, randomised placebo-controlled trial based in Western Australia investigated the use of 0.01% atropine in 6-16 year olds with proven myopia progression. Of the patients, 49% were of European (White) ancestry, making this the first such study to report on this ethnicity. Previous large, randomised studies were Hong Kong’s Low-Concentration Atropine for Myopia Progression (LAMP) study, Singapore’s Atropine in the Treatment Of Myopia (ATOM) study and India-ATOM.
At two years, there was no statistical difference in outcomes with spherical equivalent and axial length progressions of -0.64D and 0.34mm in the atropine group and -0.78D and 0.38mm in the placebo group. Possible explanations included placebo group drop-out of progressors after 18 months, as well as a slightly older age group which may have naturally slower progression. Sub-group analysis found slowing up to 18 months for European patients not sustained at two years but no difference at any time point for East or South Asian patients (40% of patients). Analysis of younger vs older patients similarly failed to find a difference. The drops were well tolerated.
Comment: This study indicates a possible modest benefit of 0.01% atropine for European patients but not for Asian patients. In the larger LAMP2 study based in Hong Kong (Yam JC et al, Ophthalmology 2020), 0.01% atropine had a progression after two years of -1.12D and 0.59mm – nearly twice that of this study. Environmental and country specific modifiers may play a role. Further studies are needed to investigate higher doses of atropine (0.025% and 0.05%) in non-Asian patients. Comparison studies of atropine vs myopia control glasses vs orthokeratology contact lenses are also lacking.
Oral fluorescein angiography for the diagnosis of papilloedema versus pseudopapilloedema in children
Elhusseiny AM et al
American Journal of Ophthalmology 2023:245;8-13
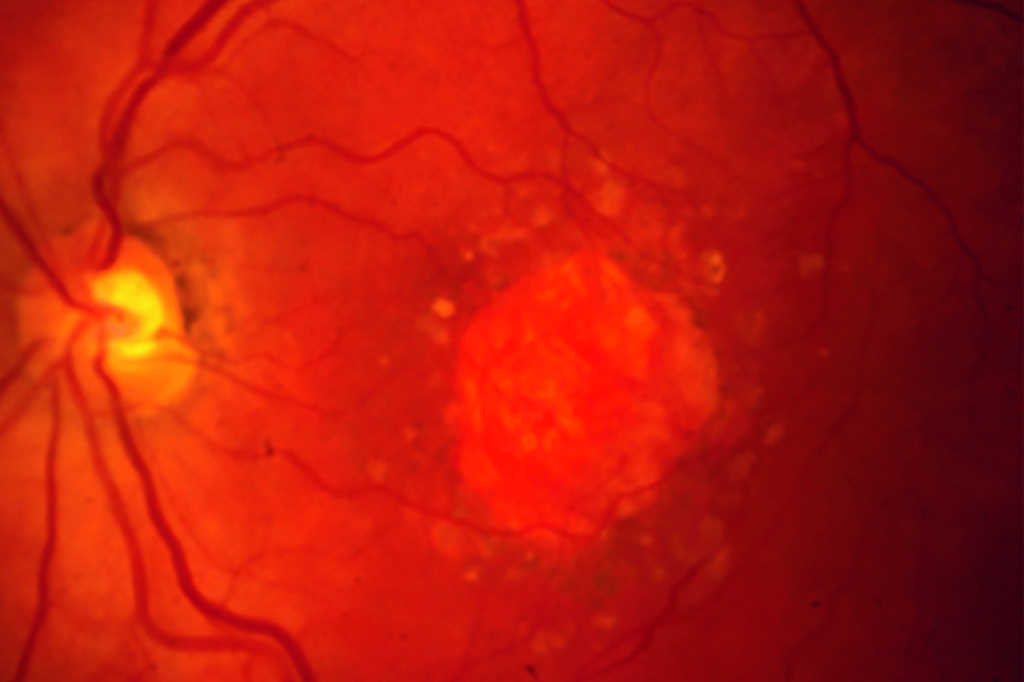
Review: This retrospective study investigated the accuracy of oral fluorescein angiography in distinguishing papilloedema (n=11) from pseudopapilloedema (n=34) in paediatric patients. Two masked specialists analysed imaging for leakage from the optic nerve head, a feature seen in true papilloedema. The accuracy of the test compared to the final diagnosis was 62% for reviewer one and 69% for reviewer two. The negative predictive value was 90%, meaning pseudopapilloedema could be correctly identified 90% of the time.
Comment: Oral fundus fluorescein angiography in children has been performed in Auckland since 2022 and provides an easy and pain-free method of obtaining high-quality images in children with vitreoretinopathies.
Swollen optic nerves in children is a frequent and challenging referral to the paediatric eye clinic from optometrists. Despite detailed history, examination and optic-nerve imaging, for some cases the only definitive diagnostic method is magnetic resonance imaging (MRI) brain and lumbar puncture, which often entails a general anaesthetic. An investigation which could reliably and expediently diagnose patients within the eye clinic would be of huge benefit both for early diagnosis for the family and to reduce repeat visits and investigations.
Unfortunately, fundus fluorescein angiography is not the answer – particularly for mild papilloedema, which presents the largest diagnostic challenge in clinic – but a negative test provides useful information.
The paediatric optic neuritis prospective outcomes study: two-year results
Pineles S et al
Ophthalmology 2022;129(8):856-864
Review: This non-randomised, two-year observational study in 23 worldwide clinics prospectively followed children diagnosed with optic neuritis (ON) to accurately ascertain visual outcomes, recurrence risks and final diagnosis.
Follow-up was completed by 28 of 44 children (66%), 46% of whom were female and 68% unilateral. Median age of presentation was 10.3 years (range: 5-15) with mean presenting vision of 0.81 logMAR improving to 0.14 at six months, which was sustained at 0.11 logMAR at two years. Isolated optic neuritis was found in 39%, with the remainder associated with systemic neurological conditions including myelin oligodendrocyte glycoprotein (MOG)-associated demyelination (29%), multiple sclerosis (14%), neuromyelitis optica spectrum disorder (11%) and acute disseminated encephalomyelitis (ADEM) (7%). Two patients had recurrence in the same eye and two had recurrence in the contralateral eye. All patients had corticosteroid treatment. Two of 12 initially diagnosed with isolated ON were found to have associated disease.
Comment: This study aimed to fill a gap in the literature on prospective studies in paediatric ON. It provides useful information for counselling on visual outcomes as well as for directing systemic workup. It suggests that in children, a large proportion of patients have systemic neurological conditions but those presenting with isolated ON are unlikely to develop associated disease. Most demonstrated good vision recovery by six months. However, the small numbers due to low recruitment and large drop-out limit firm conclusions.

Dr Sarah Hull is a specialist in paediatrics, strabismus and genetics, working at Te Whatu Ora Auckland and Auckland Eye, and a senior lecturer at Auckland University.