RANZCO NZ 2018: Conference report
The 2018 RANZCO New Zealand branch annual scientific meeting was held in the heart of Auckland city, at the Hilton Hotel from 11-12 May. Incorporating parallel conferences for the New Zealand ophthalmic nurses and Orthoptic Society (see separate stories) delegates from across New Zealand, Australia and further afield attended to enjoy the exciting programme.
As we have become accustomed to, this year’s programme again boasted a strong clinical and scientific line-up, featuring an array of both national and international specialists, including Professor David Mackey (Australia), Associate Professor Lyndell Lim (Australia), Professor Brendan Vote (Australia) and Helen Gibbons (Moorfields Eye Hospital, UK) to name a few.
The meeting started on Friday morning with the plenary session in which all four of the keynote speakers shared a portion of their knowledge by providing the latest updates in their respective fields.
Genetics, uveitis and visually-impaired simulation training
Prof Mackey led the session with a thought provoking presentation ‘Eye genetics at the fork in the road’. Giving a brief synopsis of the history of genetic research and major discoveries to the present time, sharing the evolution of gene-based therapies and touching on the future, where decisions will need to be made on how we channel limited funding to best improve patients’ lives in a society of expansive genetic research and interventions.
Prof Vote, carried on the genetics theme with ‘Ignore what you’ve learned, it’s time to run with the scissors! CRISPR-cas 9”. He outlined the current state of CRISPR research and gene therapy, highlighting that Australia and New Zealand have some of the world’s leading researchers in the field. A/Prof Lim went on to share her expert pearls of wisdom on maximizing post-operative outcomes and avoiding potential pitfalls when operating on uveitis patients with cataracts.
Helen Gibbons completed the morning with a great presentation, offering the audience some insight into the specifics of visual awareness training, including simulation exercises, nurses are exposed to as part of their ophthalmic training at Moorfields. The training sessions, Helen explained, are invaluable for patients as the nursing staff gain an intimate understanding of the struggles, fears and challenges their patients experience on a daily basis.
A brief look at the orthoptists' and nurses’ meetings
Following morning tea, the programme split into three. The orthoptist sessions included a fine line-up of some of New Zealand’s leading neuro-ophthalmologists presenting an array of interesting cases and stimulating a good string of discussion. In the nurses’ meeting, Dr Dianne Sharp discussed the challenges we are faced with, given our ageing population in her presentation: ‘Macular degeneration in the ageing eye: understanding the pathogenesis and optimising treatment outcomes’. Here she touched on the responsibility we had in educating the public on signs and early treatment, and the recent development of RANZCO’s referral screening pathway (see separate story) to assist with the management of this condition in the community to decrease the potential burden. The concept and importance of ‘working as team’ to implement paths to achieve the best visual outcomes for patients was a strong point made here. See separate stories for more on the orthoptists and nurses meetings.
Technology claims, genome studies, 3D mapping and more on uveitis
The main scientific programme’s afternoon sessions began with a talk by Prof Vote: ‘Would you like fries with that? Upselling cataract surgery and a doctor’s role in emerging technologies.’ Here, he highlighted the importance of being an ‘enthusiastic sceptic’ in face of the ever-expanding release of new technologies in the surgical world, taking the audience through an interesting history of his own research experience over the years in the face of such changing technologies.
Prof Mackay followed with an overview of the genome-wide association studies, the identification of dozens of genes associated with POAG, intraocular pressure and optic disc parameters, and next-generation sequencing, identifying genes associated with congenital and developmental glaucoma. Several genes, he explained, were being identified in both disease subgroups, suggesting that congenital glaucoma and POAG may both be part of a ‘spectrum of disease’ rather than distinct clinical entities.
Auckland-based Dr David Squirrell completed the session with ‘3D mapping of the retinal and choroidal circulations. A novel representation utilising swept-source OCT angiography’. He presented algorithms developed by his team that produce highly-detailed 3D maps of both retinal and choroidal circulations. These advances, he explained, have the potential to further the understanding of the pathophysiology of visual loss in retinovascular diseases.
The first day’s educational sessions came to completion with A/Prof Lim’s ‘The rise and rise of infectious uveitis – The usual suspects: herpetic anterior and posterior uveitis and toxoplasmosis’. She provided a synopsis of the basic principles of recognizing uveitis and discussed the latest knowledge in managing common causes of infectious uveitis. The remainder of the final session was filled with an array of cases and research from across the country, giving the audience a taste of the emerging talents within ophthalmology in New Zealand.
The conference dinner
The fun continued into the night with this year’s conference dinner held at the Maritime Room on Princes Wharf. The relaxed, informal dinner was a novel and enjoyable experience. The ‘street-style’ cuisine was delightful, both in presentation and flavour, and the casual environment enabled much mingling.
MD and the pros and cons of being outside
Highlights from Saturday included the plenary session where Prof Vote started the day off with, ‘Til death do us part! Lessons from my 10+ year macular degeneration relationship’, where he presented results from his research projects, illustrating how far we had come in the last 10 years with the ‘intravitreal injection revolution’.
Prof Mackay discussed ‘Outdoor activity and myopia, risks and benefits’, presenting some fascinating data on the importance of kids spending time outdoors in the fight against myopia versus the cons, such as pterygiums and skin cancer. This was a particularly important point for our part of the world, which is known to have the highest rates of cutaneous melanoma in the world, as pressure increases for children to spend more time outdoors to combat myopia.
Helen Gibbons and A/Prof Lim rounded off the session, with Gibbons’ presentation, ‘Advanced practice roles in Moorfields’ and Lim’s essential points of ‘Cataract Surgery in patients with diabetic macular oedema’.
NZ’s role in emerging ophthalmic ideas
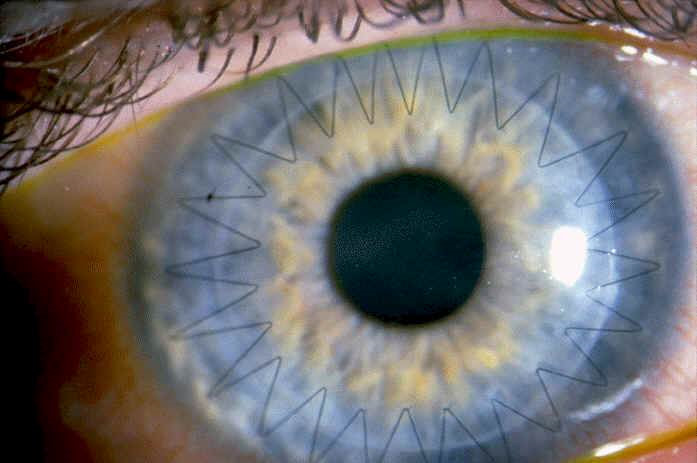
The following sessions showcased more emerging concepts and technologies in ophthalmology and ophthalmic sciences and New Zealand’s role within these. Presentations of note included University of Auckland ophthalmology chair, Professor Charles McGhee’s ‘Keratoconus approaching 2020: this is not the end but it may be the beginning of the end’, in which the battle against keratoconus in New Zealand appears to be progressing strongly; and Auckland University Professor Trevor Sherwin’s ‘Sex, self and stem cells’. Here, Prof Sherwin presented the preliminary results from studies analysing stem cells’ ability to form ‘stem cell spheres’ with the use of time-lapse microscopy, analysing the potency and interactions of spheres placed on collagen surfaces. The suggestion from early results being that the source of the stem cells, is likely to have some impact on the subsequent success or failure in the recipient, with there likely to be a preferential bias towards cells with the same gender lineage.
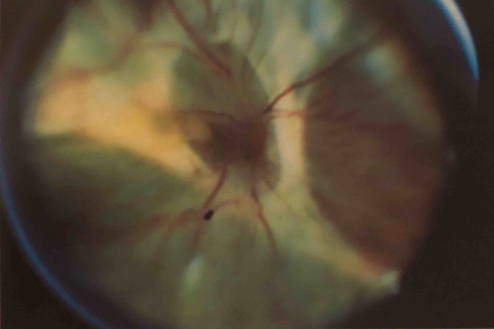
The final stages of the conference came to a close with a delightful bang. Salim Ismail presented the award winning short clip, ‘Walking with dying spheres or die another day: The journey of a stem cell sphere to fulfil the promise of regenerative medicine’. This entertaining film, part James Bond, part David Attenborough, showed time-lapse imaging of the recruitment of cells into stem cell spheres and their subsequent migration, division and potential differentiation as they repopulate a given substrate. The footage, in an extremely entertaining way, demonstrating a potential surgical tool in the treatment of corneal diseases, such as limbal stem cell deficiency. It was, yet again, another fine example of the quality or work being produced from right here in our neck of the woods.
Concluding comments
Overall this was yet another very informative and enjoyable conference, as I often find the New Zealand Branch meetings to be. The organising committee managing again to bring together a forum of both extremely high calibre and interesting international and national guest speakers. There was a great range of clinical topics and good balance of senior and junior participation at what turned out to be a record attendance.
As a whole, the 2018 meeting left me with a thought: the understanding of the complexities of the eye has moved in leaps and bounds over the last decade, all of which has, in some way, impacted directly on our clinical practice. I stand in awe of how fortunate we are, that in this small part of the world, such a high calibre of clinicians and scientists are not only pushing the boundaries of our knowledge, constantly, but also sharing the concepts so that our scope of clinical care is forever improving the visual outcomes of the communities we serve.
About the author
Dr Kaliopy Matheos is in her final year of training, having recently completed her part 2 examinations. She is currently the ophthalmology registrar at Tauranga eye clinic.