RANZCO’s ophthalmology 2030: more equity, advanced technologies
Despite being postponed and having to reinvent itself as a virtual meeting, the much-anticipated RANZCO 52nd Congress was a huge success. Before getting into the fantastic sessions, I’d like to acknowledge and commend the conference organisers and team, who did an amazing job arranging four days of engaging scientific lectures into a user-friendly and interactive online platform.
The agenda had something for everyone, with topics ranging from RANZCO’s Vision 2030 plan, sustainability within ophthalmology, ensuring equity of access to the various uses of artificial intelligence (AI) in ophthalmology, gene therapy, master courses and much more.
Day 1. Equity, genetics and best papers
The opening session launched RANZCO’s Vision 2030 and Beyond plan. It aims to ensure equitable access to eye healthcare and eliminate avoidable blindness in Australia, especially given that 90% of permanent visual impairment and blindness is preventable. RANZCO president Professor Nitin Verma together with Dr Kristin Bell, Dr Justin Mora, Associate Professor Ashish Agar and Dr Philomena McNamara presented the college’s Vision 2030 plan, proposing solutions to access and care inequity. The maldistribution of outpatient services in Australia has significant ramifications for patient populations, they said, highlighting one proposal to develop an Atlas of Healthcare Delivery Standards to enable local stakeholders to address local population needs.
This was a fascinating and commendable array of talks demonstrating RANZCO’s vision for the future and its commitment to improving equity of care. The Vision 2030 model could also be adapted to address issues of inequitable access to care in New Zealand. With the plethora of highly cost-effective interventions that exist today, preventable visual impairment and blindness should be a thing of the past.
Professor Alex Hewitt, from the Menzies Institute for Medical Research in Tasmania, delivered this year’s Dame Ida Mann Memorial Lecture, ‘The dawn of precision ophthalmology in the Asia-Pacific’. He discussed the use of gene editing technology, specifically CRISPR. Genetic testing and technology can now be used to diagnose, design and validate genetic correction therapy. Prof Hewitt was not alone in using the editing tool, with several other presenters during the congress also discussing their use of CRISPR. In line with the Vision 2030 theme, there is a need to ensure equity of access for all for this and other emerging technologies, given the positive prospects for patients who have access to them.

Prof Hewitt
Next up was the best paper session with the John Parr Trophy and Gerard Crock Trophy award winners. The developing use of technology was a running theme among some of the best papers. Auckland-based medical student Finley Breeze, winner of the John Parr Trophy, discussed how machine learning algorithms may be used to target and improve clinic attendance appointments. Although approaches such as text-reminder services exist, machine learning algorithms may help us target patients who are more likely to not attend appointments.
Auckland-based Dr Joevy Lim presented a review of the incidence and mortality of ocular melanoma in Aotearoa over 21 years. This large retrospective study identified an age-standardised annual incidence of 6.97 cases of ocular melanoma per million per year with median survival time from diagnosis of 10.1 years. Next, Sydney Eye Hospital’s Dr Jason Daley discussed the development of a deep learning algorithm for a south-west Sydney diabetes retinal screening service. He highlighted the unmet clinical need for such a service and how AI can be used to fill this need.
Clinical lead for New Zealand’s diabetic eye screening programme, Dr David Squirrell presented a multicentre prospective evaluation of Theia, a New Zealand-made bespoke AI system developed to improve the detection of diabetic retinopathy and diabetic macular oedema in large patient populations. Widespread use of this within the New Zealand diabetic screening programme would increase overall screening capacity and reduce costs per unit screen. I look forward to seeing how this develops!
In other papers, Auckland-based optometrist Dr Samantha Lee presented on the incidence and progression of myopia in 20-28-year-olds and the risk factors for myopia onset and progression in young adulthood; and Melbourne-based ophthalmologist Dr George Kong, winner of the Gerard Crock Trophy, shared 12-month outcomes in monitoring glaucoma patients using a tablet. Clinic-based visual field monitoring for glaucoma patients can be resource intensive, but devising a simple, home-based monitoring system has the potential to allow for earlier detection, improved compliance and improving services overall, he concluded.
Day 2. Cataract surgery and sustainability
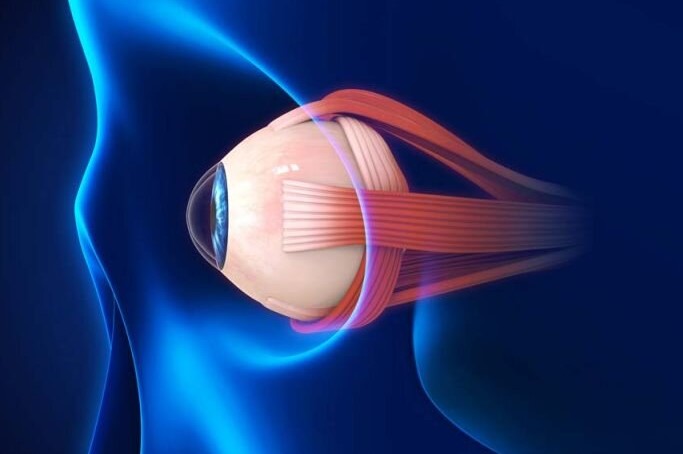
Cataract surgery remains the most commonly performed ophthalmic surgery worldwide. Understanding the intraocular lens (IOL) formulae and when to apply them is critical to providing patients with the best possible outcome. This theme was kicked off during the Bausch & Lomb-hosted morning symposium. Well-known Perth-based ophthalmologist and researcher Professor Graham Barrett, this year's Norman McAlister Gregg Lecturer, ended this session discussing how and when to treat low levels of astigmatism.
Glasgow-based cornea and anterior segment specialist Dr David Lockington presented an engaging and entertaining Cataract Update Lecture. This focused on ensuring a safe cataract experience for all by embracing simulation for teaching and training and thus avoiding the perils of the ‘Beyoncé method’ – who knew the jelly Destiny’s Child was singing about was of the vitreous kind!

Dr Lockington
The day continued with the RANZCO plenary and ORIA plenary sessions. Wellington-based ophthalmologist Dr Jesse Gale chaired a stimulating session on sustainability and provided suggestions on how to improve our carbon footprint, professionally and personally; while guest lecturer Dr Cassandra Thiel reminded us to rethink, reuse, reduce and recycle. Applying these four Rs to our daily lives could go a long way towards improving sustainability.
Day 3. Neuro-ophthalmology and an array of controversies
I enjoyed learning about upcoming medications with the potential to improve vision for patients with geographic atrophy (GA) during the first session hosted by Apellis Pharmaceuticals, which is currently investigating intravitreal pegcetacoplan for GA. As new technologies emerge, the potential to really tackle the macular degeneration disease burden continues to improve.
Next up, Professor Lynn Gordon, University of California, Los Angeles (UCLA), gave an interesting and informative presentation on advances in neuro-ophthalmology. The treatment of specific cancers has been revolutionised through the use of immune checkpoint blockades, which unleash the body’s own immune surveillance and mechanisms to kill tumour cells. However, it can result in autoimmune issues which affect the eye and central nervous system.

Prof Gordon
Providing this year’s Retina Update Lecture, San Francisco-based Professor Anita Agarwal discussed how gene testing is providing new insights into retinal dystrophies and advancing our understanding of genotypes and phenotypes. This was followed by the Council Lecture, presented by Sydney Eye Hospital’s Associate Professor Clare Fraser who returned us to neuro-ophthalmology with a series of interesting clinical vignettes, including ‘seeing stars’ in concussion and Visual Snow Syndrome, an increasingly recognised visual phenomenon which now has its own set of diagnostic criteria.
Another highlight of the third day was the expert panel who delivered some brilliant talks on clinical controversies within ophthalmology. One, introduced by Hawke's Bay-based ophthalmologist Dr Liz Insull, discussed retrobulbar hyaluronidase for filler-induced blindness. Hyaluronic acid filler-induced blindness is rare but not infrequent. Should acute eye clinics now have hyaluronidase in their arsenal? Another controversy, shared by Associate Professor Lyndell Lim, principal research fellow at the Centre for Eye Research Australia, shed light on what Covid-19 infections and vaccinations mean for some of our patients.
Day 4. Evaluating glaucoma and closing the gap
Rather than winding down, the last day of congress continued to educate and entertain. Professor Pradeep Yammanuru Ramulu, director of the Wilmer Eye Institute’s glaucoma division at John Hopkins Medicine in Baltimore, US, delivered the Glaucoma Update Lecture reviewing some more novel concepts for evaluating functional damage in glaucoma. He reminded us of the real-world consequences of glaucoma and how much it can impact a person’s life.

Prof Ramulu
The final plenary symposium, ‘Improving eye health for Aboriginal and Torres Strait Islander Peoples - equity in everyday ophthalmic practice’, highlighted some invaluable work to close equity gaps in Australia. Professor Verma encouraged us to uphold RANZCO’s mission to be advocates on behalf of all our patients and the wider community, while Professor Hugh Taylor explored collaboration and workforce needs in eyecare. This session highlighted some of the fantastic work our community is doing to reduce inequities, both in Australia and New Zealand, and clearly showed the importance of a collaborative approach to continue to foster and develop these initiatives.
Insightful access on-demand
Each afternoon session had a range of symposia, bootcamps and rapid-fire sessions. The virtual hub gave us flexibility to attend overlapping sessions. All of the courses and symposia I attended provided useful and practical guidance from experts in their fields. The rapid-fire sessions provided insights into the cutting-edge work of many of our colleagues, all supplemented with some thought-provoking question and answer sessions. These were invaluable learning sessions and I highly recommend watching them (sessions can be accessed until the end of June).
In conclusion
Bringing the main part of the congress to a close and full circle, Melbourne-based Associate Professor Catherine Green delivered the Fred Hollows Lecture, ‘Disruption and innovation: challenges and opportunities in ophthalmology’, highlighting the importance of innovation, but only if it’s made available to all. The introduction of affordable IOLs for patients in developing countries, as championed by Professor Fred Hollows, is an example of a disruptive innovation that has had a profound impact on eye health globally. It also neatly demonstrates how a systemic approach is required, with innovation not only in eyecare delivery but in policy, workforce planning and education.

A/Prof Green
This virtual conference was a tremendous success! I loved the varied format of the sessions, while the live streaming and ability to watch on demand meant you didn’t have to choose between simultaneously occurring sessions. My work WhatsApp group was filled with reminders to attend informative sessions as we swapped notes on favoured congress content. The transitional music was also upbeat and catchy; I even found myself tapping along to it! The online chat function made connecting with people easy and I used it to reach out to other speakers to follow up on their fascinating presentations and posters.
Many thanks too to the congress sponsors, many of whose symposiums, virtual exhibition booths and links to useful PDFs I enjoyed. Being able to download and save information leaflets was useful and also helped reduce my carbon footprint.
The 52nd Congress highlighted some of the incredible work being performed within our community, locally and abroad! Advancements in AI and new technologies may lead to decreased rates of visual impairment and improved quality of life for our patients, while improving equity and our own sustainable work practices will tackle inequality and create a sustainable future for all.
It is always great hearing from experts and up-and-coming researchers within ophthalmology. Whether they be in person or virtual, or a hybrid of the two, I look forward to the next conferences: RANZCO New Zealand in Blenheim, 21-23 April; and the 53rd RANZCO Congress in Brisbane, 28 October-1 November this year.

Dr Ruhella Hossain is a non-vocational registrar for the Hawke's Bay DHB and an MD candidate with the University of Auckland, supervised by Drs James McKelvie, Stephen Guest and Stuti Misra. She is one of the 2021 recipients of the Save Sight Society Heather MacKintosh Junior Researcher Award and is passionate about reducing inequities of care.