The great retina vs glaucoma specialists showdown
The first Eye Institute optometry seminar for 2025 eschewed the usual format of guest lecturers and quickfire presentations of unusual cases in favour of a more relaxed and entertaining wrestling match between Team Retina (the Detachments) and Team Glaucoma (the Pressure Cookers).
The Detachments were led by Dr Narme Deva with Drs Will Cunningham and Kevin Dunne in support. Limbering up in the Pressure Cookers corner was Professor Helen Danesh-Meyer, with Drs Kaliopy Matheos and (fresh off the plane from Malta) Graham Reeves also weighing in. Dr Jay Meyer kept the showdown clean but with sufficient levity to make for an entertaining and very fast moving evening.
Before the first blows were struck, Dr Deva made a presentation to optometrists Malcolm Lowry and Kenny Wu in celebration of their progression through the first training programme for accreditation for performing YAG laser capsulotomies.
Steroids – cure or culprit?
According to Dr Deva, retina specialists and glaucoma specialists do not always share the same perspective on the use of steroids, the wonder drug with so many side effects.
Steroids are used throughout the body to fight inflammation. They calm the drama, put out fires and are used in everything from routine cataract surgery post-operatively to treating sight-threatening uveitis. They’re also used for diabetic macular oedema and as an adjunct to anti-VEGF treatment. Since steroids prevent tissue damage and scarring, they also preserve vision.

Anton Frank, Helen Heyns, Sasha O'Sullivan, Kevin Wong, Tim Chang and Run Tung Li
Team Retina maintained that, since even low-grade inflammation in the eye can lead to irreversible structural damage over time, accepting inflammation is accepting the potential for long-term visual compromise.
However, 30% of the population are known to be steroid responders. Just a hint of steroid in the eye from drops or periorbital creams, up the nose as nasal spray, systemically to reduce immune response or even, according to Dr Meyer, after an injection into an aching joint, can cause an increase in intraocular pressure (IOP) in a steroid responder.
Cataract surgery with any history of inflammation becomes more demanding and the results less predictable, so cataract surgeons will reach for the steroids well before they operate, with post-operative control of inflammation key to success. It is reported that cystoid macular oedema (CMO) occurs in 30–56% of eyes post-operatively. The risk can be reduced by careful control of pre-operative inflammation with corticosteroids, as well as observing a period of inflammatory quiescence of at least three months post-operatively.

Joseph Stone, Lisa Ang, Dian Zhuang and Sophia Tan
Team Glaucoma performs under pressure
Glaucoma patients and steroid responders need rescuing and protecting from steroid-splashing colleagues, responded Prof Danesh-Meyer’s team. Most at risk are young patients, particularly children, who often show a higher sensitivity to increased IOP from steroids. Also at risk are those on long-term treatment for eczema, asthma or chronic allergies with prolonged use of oral or topical treatment.
Steroid challenge testing, such as allergy testing, with a topical or periocular exposure recommended before long-acting use. Patients being given topical steroids for the first time should have their IOP checked at 7–10 days, then every two to four weeks. It is also possible to become a responder later in life, particularly if chronically on steroids.
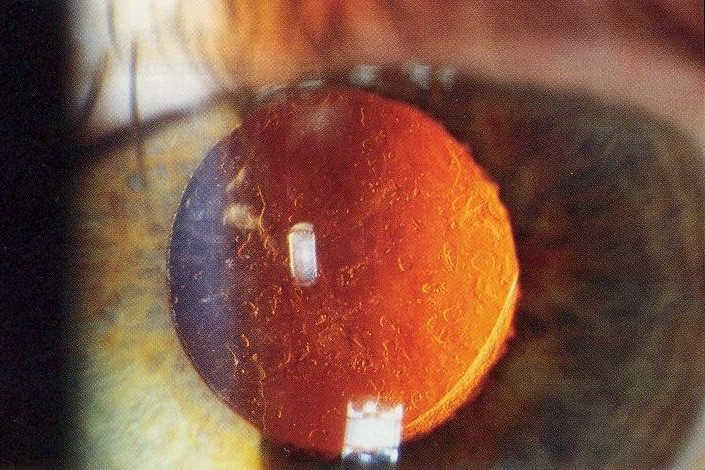
Steroids can not only push up IOP but also aid cataract formation. The incidence of steroid-induced cataracts is 68.1% with topical use and 22.5% with prolonged oral or intravenous use.

Teresa Fleming and Amanda Smit
The good news is that only 5–6% steroid responders show a marked increase of IOP after 4–6 weeks of topical steroid use, though this can occur as soon as 7–10 days after commencing treatment. The bad news is that stopping steroids does not always fix the problem.
The take-home message was to know your glaucoma patients and those who may be at risk of elevated IOP. Do not assume anything, ask plenty of questions about long-term medications – even over-the-counter treatments for allergies. Monitor IOP, even in children, and communicate with GPs, ophthalmologists and most of all with the patient themselves. Steroids make people feel better and more comfortable so they tend to keep using them and, unaware of the risks, GPs will often keep prescribing them.

Karthigan Paramananthasivam and Dr Graham Reeves
Team Glaucoma members said they stand by to manage the situation by either discontinuing steroids (not always possible), removal of depot steroids (vitrectomy may be considered) or ultimately treat the glaucoma, which is much like treating primary open-angle glaucoma.
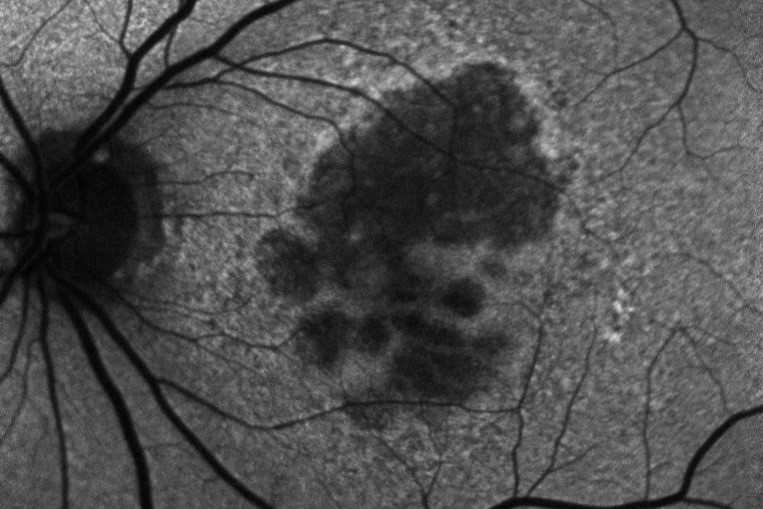
Other topics covered during the presentation were diabetic retinopathy (DR) and neovascular glaucoma. The key to the management of DR, according to Dr Dunne, is the systemic management of diabetes, feeding the information on retinal changes back to the GP with recommendations for monitoring HbA1c, regular retinal screening and patient education. This includes showing patients the evidence of damage in the eyes caused by their diabetes and pointing out that this damage is happening elsewhere, even if we can’t see it as readily as in the eyes.
Once again, in the tussle between DR and neovascular glaucoma, collaborative care is the winner. Is it better to first drop the IOP or give the anti-VEGF injection? If high pressure is driving the ischaemic response, drop the pressure first. Once the eye is entered, the danger of pressure spikes, ropey vessels and other adverse events is increased.

Kyla Kubba, Rebecca Kassir and Dr Kevin Dunne
A key message was to advise patients’ medical teams that dropping the HbA1c too quickly is dangerous and can lead to retinopathy blowing up.
Prof Danesh-Meyer delivered a frightening list of systemic side effects of beta blockers and how to avoid adding to these issues in glaucoma patients. Her parting shot was that a lot of damage is hidden in glaucoma. Glaucoma specialists look for the invisible and fight the unknown, which makes them different from retinal specialists. Ultimately though, they all “need to work so patients are seeing until they leave this Earth”.
The last word went to Dr Meyer who simply said, “As a glaucoma specialist, the worst part of the job is the pressure you always have to deal with!”

Naomi Meltzer is an optometrist who runs an independent practice specialising in low-vision consultancy. She is a regular contributor to NZ Optics.