Eye Doctors provide a warm start to autumn
The arrival of autumn heralds the Eye Doctor’s first Grand Round of the year. Held at the Novotel in Ellerslie, Auckland, this year’s inaugural seminar on 28 March was a warm and welcoming affair with many local optometrists attending keen to kick off their annual cpd hunt and hear the latest surgical updates from Eye Doctors’ surgeons.
Wobbly eyes
Paediatric eye specialist, Dr Shuan Dai kicked-off proceedings this year with a talk about childhood nystagmus or “wobbly eyes”, a disorder distinguished by involuntary eye movement. He presented examples of different types of wobbly eyes, explaining how to reach the correct diagnosis, which is important not only for treatment but because the disorder can be a sign of something more sinister, like multiple sclerosis or a brain tumour, requiring further investigation such as neuroimaging.
When the condition is associated with photophobia or vision loss, this can be caused by albinism, aniridia, retinal dystrophies, Leber's congenital amaurosis, optic atrophy/hypoplasia, foveal hypoplasia and retinopathy of prematurity (ROP). Occasionally, systemic conditions such as ataxia (acute onset) and hydrocephalus can cause nystagmus.
Dr Dai told the audience if you suspect nystagmus in a patient with normal ocular examination results, remember “in medicine, nothing comes in isolation”, you need to look for other symptoms and patterns, such as laterality (monocular must exclude central nervous systems gliomas), jerk/pendular, horizontal/vertical/mixed movements, amplitude, frequency and other abnormalities such as head nodding to direct you to the likely diagnosis and further investigations.
After establishing the reason for the nystagmus and making a full diagnosis, including any link to secondary central nervous system diseases, managing the patient includes offering treatment of amblyopia, low vision services and, possibly, nystagmus surgery.
Ditch the lingo
Next up, Dr Andrew Riley took to the podium on a mission to stop what he calls our “secret language”, or using medical terminology when prescribing.
With 396 recognised abbreviations, it’s no wonder patients and sometimes even pharmacists and doctors get it wrong when eye health professionals discuss conditions using a series of ophthalmic acronyms, argued Dr Riley. Worryingly, according to some statistics presented, 20% of all medical negligence treatment claims result from the incorrect use of a treatment drug and that can result from simple miscommunication.
There are guidelines available on good prescribing practice from the New Zealand Medical Council, said Dr Riley, admitting sometimes he too was guilty of too much lingo, but if you follow the guidelines and write in plain English, using for example “every second day” rather than QOD (que otra dia), this will help reduce errors. If the prescriber, the patient and the pharmacist can read the script fewer errors will occur.
Computer-derived scripts are also helping to solve the miscommunication problem, he said, as well as better patient knowledge through improved education, familiarity with the therapeutic goal and the drug in question, plus ongoing monitoring of side effects and adverse events.
In summary, you need to get the five rights, right: the right patient, the right drug, the right time, the right dose and the right route, he said, and if in doubt, ask!
Glaucoma drops and complications
After a short break, Dr Mark Donaldson shared three cases illustrating how different glaucoma eye drop treatments can cause unexpected and undesired complications.
One case involved a myopic, 70-year-old engineer who presented with suspected cystoid macular oedema (CMO), after post-operatively using a topical prostaglandin analogue/beta-blocker combination.
The patient had been treated for epiretinal membrane left eye vitrectomy in 2014. He had open angle glaucoma. The concern was the patient’s intraocular pressure, said Dr Donaldson, which was why beta-blockers were prescribed. But the patient’s vision began deteriorating. Test results showed that CMO, which is statistically associated with post-operative use of topical PGAs - relative risk (RR) 1.86, 95% CI 1.04 to 3.32 and topical beta-blockers (RR) 2.64, 95% CI 1.08 to 6.49.
The post-operative use of each bimatoprost (RR 2.73, 95% CI 1.35 to 5.53%) and travoprost/travoprost/z (RR 3.16, 95% CI 1.42 to 7.03) in the year prior to diagnosis had been shown to have a statistically significantly association with the prevalence of pseudophakic CMO. This association, however, said Dr Donaldson, was not observed to be statistically significant with the post-operative use of latanoprost (RR 1.55, 95% CI 0.84 to 2.88). Interestingly, however, his patient responded to having the hysite (latanoprost) stopped.
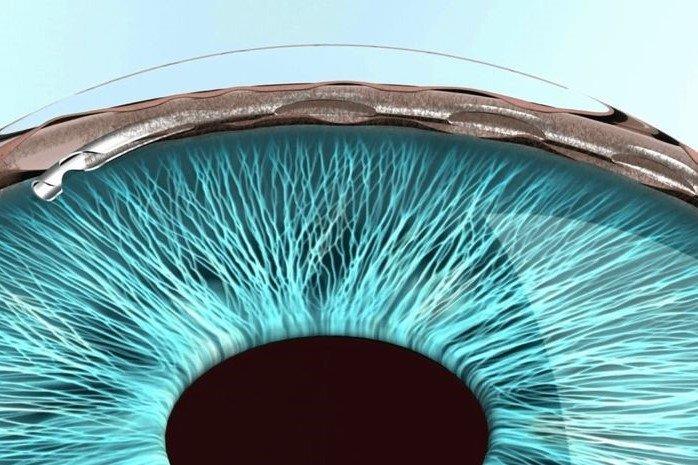
Pterygium surgery
Pterygium surgery has come a long way in recent decades, said the final presenter of the evening, Dr Penny McAllum, with surgeons changing to techniques providing lower recurrence rates, such as conjunctival autografting with a 2-18% rate of recurrence. This compares with the old-school, five-minute scraping the sclera process which resulted in up to a hefty 88% recurrence.
There is also a method called P.E.R.F.E.C.T, Dr McAllum said, now considered the gold standard in some centres, with reported recurrence rates of less than 0.1%. So far, this procedure (pterygium extended removal followed by extended conjunctival transplant) has been successfully carried out in Australia and comparable results have been shown in a recent European study.
To further reduce recurrence, Dr McAllum said she prefers tissue glue to sutures. When used correctly, a meta-analysis shows it reduces the recurrence rate by 47% due to less postoperative inflammation, she explained.
The main problem with current surgery is the lack of standardisation in and recording of the techniques used and the resulting outcomes, she said, adding that there was a healthy debate on the topic at the recent Australia and New Zealand Cornea Society meeting (see NZ Optics' April issue). Some surgeons, who have developed a new surgery technique, using a femtosecond laser to harvest the conjunctival graft, are suggesting this will improve results by avoiding undertaking a technically challenging part of the surgery manually. A point Dr McAllum explained using the analogy, “if you’ve got a hammer, everything will look like a nail”.
With proper training and standardising measured cosmetic and medical outcomes, pterygium surgery results will continue to improve, she said, ending the evening on a resounding upbeat note.
The next Eye Doctors’ Grand Round will be held at Ormiston Hospital on 13 June by invitation only, given space constraints, while the final Grand Round for the year will be held on 31 October.