Regarding the retina
The first of the two-repeated autumn seminar evenings by Retina Specialists was held on 6 March in the leafy Auckland suburb of Parnell. Attending optometrists were greeted by the Retina Specialists team, wine and canapés.
The all-female speaking line-up for the evening included Retina Specialists’ Dr Rachel Barnes, Associate Professor Andrea Vincent, Dr Dianne Sharp and Dr Narme Deva.
A pictorial FAF journey
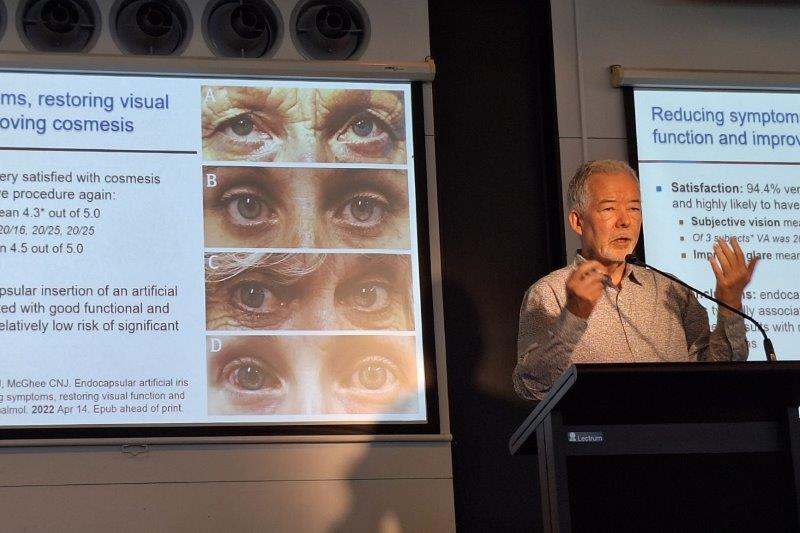
A/Prof Vincent kicked off the evening with a pictorial journey through fundus autofluorescence (FAF) in clinical practice, showing us “pretty pictures” depicting the presentation of various retinal dystrophies and disorders. FAF is a non-invasive technique, which highlights lipofuscin (the main fluroflore in the retinal pigment epithelium). FAF may detect abnormalities beyond the clinical exam and is useful in classifying various retinal dystrophies and disorders, she said.
In albinism, where the retina is not metabolically affected, the FAF appears normal. However, in choroideremia (an X-linked retinal condition affecting males) widefield Optos images show patchy changes with scalloped edges where the retina is ‘metabolically dead’. In X-linked retinitis pigmentosa there is a so-called water-shed zone seen between the good and bad metabolic areas of the retina. In PDE6B retinitis pigmentosa, FAF is very useful - visual results are closely correlated to FAF, so generally visual fields are not necessary and don’t give any extra information, A/Prof Vincent explained.
Among other fascinating pearls, Vincent also revealed what she calls the ‘moustache sign’ of the adRP rhodopsin mutation - an inferior central rim of hyperfluorescence - and showed FAF images of eight siblings with different presentations of ABCA4 retinal dystrophies, where the whole retina may be affected.
AMD new treatments?
Dr Barnes spoke about the new treatment options for age-related macular degeneration (AMD). She begun her presentation by outlining the goals of the different treatments for both dry and wet AMD, and enthusiastically explained what else waits in the wings in the long journey to market.
The first drug she discussed, Roche’s lampalizumab, an antigen-binding fragment of a humanised, monoclonal antibody directed against complement factor D (CFD), had showed promising initial results in early trials with a 20% reduction in geographic atrophy. The phase III results, however, showed no benefit at all. Nano-second laser may also have an application in early dry AMD, with pilot studies indicating a reduction in drusen. Phase III results are expected later this year.
Looking at possible treatments for wet AMD, Barnes reminded us gravely that there is no permanent cure for this devastating disease and that real-world results often fall short of drug trials due to under treatment. A new pigment-derived growth factor, which it was hoped would work to reduce fibrosis and help mature vessels to regress, looked hopeful early on but was ineffective in phase III trials. Roche, however is still in the game, with its drug, also based on angiopoitein (a proangiogenic cytokine involved in neovascular AMD), and is persevering with the expensive trials required.
A new formulation of ranibizumab (Lucentis: a recombinant humanized IgG1 monoclonal antibody fragment that binds to and inhibits vascular endothelial growth factor A) delivered by a port system is also an exciting possibility with more results planned soon, said Dr Barnes. Gene therapies using new viral vectors are also being trialled. While many trials seem to show early promise and then fall at the final hurdle, brolucizumab is in Phase III trials and results are looking very positive. With its small molecule size allowing higher potency in the eye, results are showing significant reduction in retinal thickness and better performance than aflibercept (Eylea), she said.
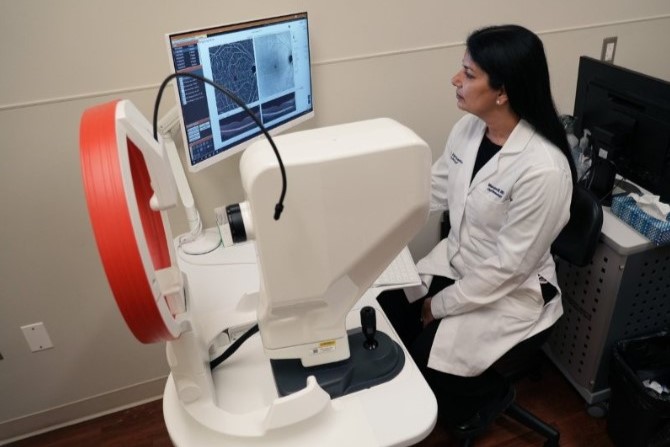
Lastly Dr Barnes discussed the new imaging technique, OCT-A that offers a quick, non-invasive 3D method to image the retinal vasculature. It is particularly useful for showing the structure of choroidal neovascularisation and for visualising occult neovascularisation not visible by any other means, she said.
MD and the ageing eye
Dr Sharp presented a practical presentation on MD in the ageing eye. The high metabolic demand of the macular area of the retina makes it particularly susceptible to oxidative damage, she said. With more than 10% of babies born today destined to become centenarians, MD is more relevant today than ever.
A recent model-of-care, commissioned by the government, highlighted the national low understanding of the disease and areas requiring improvement, such as speed to treatment. This model set out the importance of prompt care and said the time from first diagnosis to first treatment should be no more than one week. The Beckman classification can be used to identify different stages of AMD and help to predict the risk of progression at each stage, she said.
“Small fine drusen (or druplets as they are sometimes called) are not MD and it is wrong to call them this. Soft drusen combined with pigment changes are high risk. Give the patient an Amsler Grid test and monitor them closely.” Those with choroidal neovascularisation can particularly be helped by getting them treatment fast, she added.
Dr Sharp also shared some data from UK records over a 12-month period, showing that the starting vision level is of great importance. Optometrists present were also interested in discussing RANZCO’s revised referral pathway for MD. “Too often a patient stops attending appointments after anti-VEGF treatments because their vision is good, only to have problems reoccur,” said Dr Sharp, providing examples of the sequelae of neovascular MD. Patients must be educated that this is a chronic disease that requires long-term management, she stressed.
DR, risks and treatment
Dr Deva tackled diabetic retinopathy, a main cause of the blindness in working-age people. One third of diabetics will have retinopathy and for a third of those it will threaten their vision. To reduce risk during the early stages, optometrists must ask about how well patients are controlling their blood sugar levels, she said, citing data that intensive therapy, reduced the risk of developing retinopathy by 76%. A good understanding of the disease and encouraging patients to form good, healthy-eating and monitoring habits is key in these early stages.
The second question that optometrists should ask is, “how is your blood pressure?” said Dr Deva. The Wisconsin epidemiologic study of diabetic retinopathy showed that lowering blood pressure can half the risk of retinopathy. The third question centres around cholesterol levels, and while this is not as well-supported by clinical data as blood sugar levels, good cholesterol control can reduce the progression of retinopathy, she said.
Dr Deva then summarised the treatments for diabetic retinopathy and associated macular oedema focusing on lasers and anti-VEGF injections. Widefield imaging is helping us monitor treatments over time, she said. Keeping to the technological theme, Dr Deva also discussed the growing interest in artificial intelligence and the rise of studies using machines that can perform deep learning (see NZ Optics March 2018 issue, p14), “that is, showing a machine data and have it teach itself how to analyse it,” may well at some point in the future replace optometrists and ophthalmologists, analysing many data points, from diagnosis and classification to risk assessment, in mere minutes, and suggesting appropriate treatment plans.
Concluding remarks
Hilary Rayner, Retina Specialists practice manager, said the evening was a great success. “It was wonderful to see so many people at our event and we are looking forward to meeting our next group in a couple of weeks. Everyone is busy these days so we really try to make the education meetings we hold interesting and useful and we really appreciate the effort that people make to come along.”
Retina Specialists’ Spring seminar evenings will be held on the 4 and 18 September.