On course with Eye Doctors
An invitation to make my way up the meandering driveway of Remuera Golf clubhouse overlooking the rolling grassy 18th fairway was a relaxing proposition after surviving Auckland rush-hour traffic. As the afternoon golfers departed, a group of optometrists sat down to an evening of education and dinner with Eye Doctors.
Practice manager Shellene Garofalakis teed off with a quick-fire quiz, which Sandhya Mathew won with a perfect 10/10 score. Then came an acknowledgement for Dr Penny McAllum, the recipient of a recent award from Southern Cross Health Society for “exceptional patient outcomes and experience” – an award that any healthcare professional would be justifiably proud of.
An update on GA treatments
Dr Arvind Gupta teased his topic with a photo of a beautiful cherry-red spot at the macula before discussing treatment options for geographic atrophy (GA) . He pointed out that preventative measures, such as nutritional guidelines promoted as a result of the AREDS studies, are shown to most benefit low socio-economic groups. But with the current price of fish and vegetables, that benefit will surely be compromised!
The first new treatment for GA, pegcetacoplan (Syfovre, Apellis Pharmaceuticals), which gained FDA approval in February 2023, continued to show 17-30% reduction in the growth rate of macula lesions in recent studies, he said. There appeared to be no difference in long-term outcomes between monthly or bimonthly injections.
A second new treatment, avacincaptad pegol (Izervay, Astellas Pharma), is available in the US but not yet approved in Europe or the UK. There is suspicion that the rate of growth of extra-foveal lesions is reduced, but there is less effect on the slower growing sub-foveal lesions, said Dr Gupta, and a significant number of those in the study went on to develop exudative macular degeneration.
The new drugs are more viscous than anti-VEGF drugs, requiring larger gauge needles, which unsurprisingly are not well accepted, he said, leading to a drop-out rate of 25% from the trials, which is regarded as “quite high”. Overall avacincaptad pegol appears to be less helpful for those who need it most, and at US$3,000 (NZ$5,000) per vial/per person, we are probably unlikely to see this treatment any time soon.
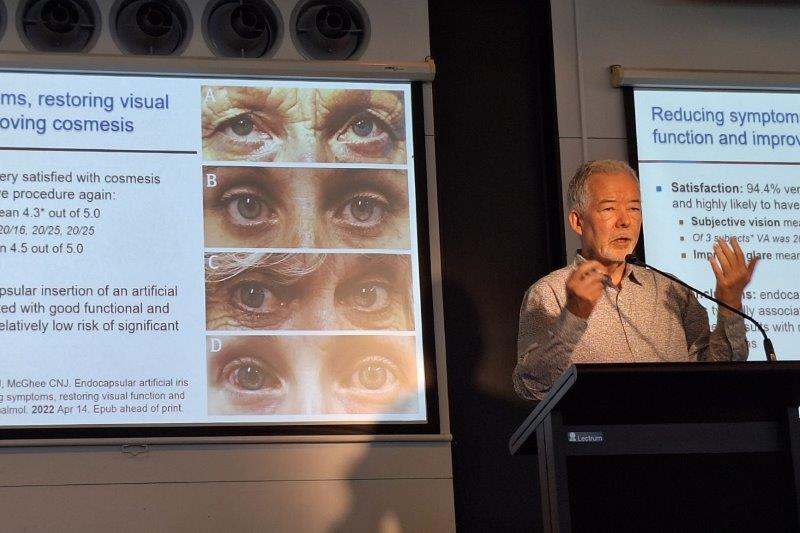
Focusing on squint surgeries
Dr Julia Escardo-Paton took a different direction by guiding us through some hard-case squint surgeries. Thinking not just outside the box, but the orbit was required for the case of heavy eye syndrome (HES), a type of myopia-induced strabismus, characterised by progressive esotropia and hypotropia – so nothing to do with an optometrist’s after-dinner posture when listening to lectures at the end of a long working day.
In one case, a 53-year-old Korean woman had binocular horizontal diplopia for more than seven years. Previously a high myope with 35mm globes, her history included previous LASIK and cataract surgeries and well-controlled glaucoma. She measured orthophoria at near and 20 dioptres esotropia at distance with diplopia. There was mild limited adduction of each eye.
HES is typically seen in high myopes when the eyes are so big they do not fit within the orbit and herniate supra-temporally. In this case, the eyes were so big that the usual tables on how much to resection the muscles to reach alignment did not really apply, which led to initial strabismus surgery failing to produce any change in diplopia. Dr Escardo-Paton noted however, that under anaesthetic this patient’s eyeballs rolled in instead of up, which gave a clue of what was to come. An MRI scan, which is usually required to confirm a diagnosis of HES, also confirmed where the muscles were and that the superior rectus (SR) and lateral rectus (LR) had splayed apart. Dr Escardo-Paton used bilateral loop myoplexies to realign the eyes. She looped a suture through the middle of the SR and LR as far back as possible and hooked the muscles together to prevent the eyes from moving forward in the globe. She did both eyes at the same time – wow! The patient awoke to cosmetically straight eyes and no diplopia for the first time in nine years, proving that strabismus surgery can be life changing. High fives all round!
Navigating medical complexities
Dr Mark Donaldson offered philosophical musings about ‘doctor speak’ and the confusion of commonly used medical terms, quoting noted author Maurice Henry Pappworth’s volume A Primer of Medicine, in which Pappworth advises doctors to think about what they are being taught.
According to Dr Donaldson, Pappworth also tackled vexing questions such as why historically the suffix ‘-itis’ was replaced by ‘-pathy’. I found this a little confusing as I thought -itis indicates inflammation, but -pathy means something wrong regardless of cause.
Out of the rough and back on track, Dr Donaldson went on to present three case histories where things were not what they seemed on first presentation. A 32-year-old Samoan man, in apparently good health and with no history of sporting or other injuries, presented to the acute clinic with pain and blurring of the right eye. His intraocular pressure was 70mmHg (right) and 20mmHg (left). Appearing as a simple case of angle closure glaucoma, the usual treatments to reduce the pressure were applied.
However, Dr Donaldson was struck by the unusual combination of a young Pacific Islander with glaucoma and decided to delve further. His hunch led to a diagnosis of diabetes with an Hba1c of 102mmol/mol presenting as angle closure due to intermittent lens swelling. A great example of if something doesn’t seem right, look right, smell right, it probably isn’t. Looking at the patient through a holistic whole-person lens, thinking about what else might be happening, paid dividends for this young man.
Can bad + bad equal good?
Dr Penny McAllum presented the case of a Tongan patient, who presented with somewhat blurry history. He’d had a stick poked into his left eye at age 8 and at 14 had fallen on to the right side of his face, damaging his right eye. On examination, the right eye had a reasonably clear cornea, but the lens appeared to be subluxated and the retina detached, a diagnosis commonly known as ‘munted’. The left eye had a dense scar across the centre of the cornea. After copious quantities of dilating drops, very little of the retina could be seen but he was able to read 6/60+, indicating the possibility of some usable vision being available if the corneal scar could be removed.
During a three-hour surgery, Dr McAllum removed the right cornea and temporarily replaced it with an artificial corneal prosthesis to plug the hole and stop leakage and entry of infection. She then removed the same diameter of corneal tissue from the left eye, finding some cataract and a very small pupil due to iris adhesion to the scarred cornea. Having cut this away and enlarging the pupil, she decided to leave the cataract for another time and stitched the cornea from the right eye into place in the left eye. The size of the graft was dictated by the size of the prosthetic plug available for the right (donor) eye. After cleaning up the scarred left cornea, she returned to the right eye to replace the plastic temporary cornea with the scarred cornea from the left eye. This right eye was not ever going to see anything much so having a scarred cornea was only cosmetic, but it was his own donor tissue in each eye which reduced the risk of rejection and long-term steroid use.
Three weeks post-op, both eyes were healing well with vision 6/30 and 6/15 pinhole. Autorefraction gave a prescription of +6.00/-2.00 cyl and the fundus of the left eye can now be seen. This lucky but accident-prone young man will see an ophthalmologist in Tonga for follow-up then Dr McAllum in a year’s time to take the sutures out with a view to left cataract surgery with a toric lens and possibly spectacles.
Challenging the anti-VEGF status quo
Moving on to the last round, Dr Andrew Riley gave a compelling argument for the use of new entries into the VEGF-inhibitors market to increase capacity and decrease cost, while still maintaining effectiveness, by challenging the current protocols for prolonged use to PRN (as long as necessary).
Firstly Zaltrap (Sanofi and Regeneron Pharmaceuticals), which is apparently aflibercept (Avastin) compounded with other agents. This has been shown to be as effective as four-weekly injections of Avastin – as long as injections start immediately and are then given at six-weekly intervals – equalling an immediate 50% decrease in the number of injections needing to be administered.
Coming soon is faricimab (Vabysmo, Genetech) which appears to be a longer lasting dual formula of VEGF inhibitors, showing superior durability and efficacy with the possibility of extension to 12-weekly injections.
If 80% of patients are maintained on a 12-week cycle, then based on 60,000 injections in New Zealand there is a potential saving of more than $30 million per year, said Dr Riley. Weighing up time and cost savings, he proposed the best combinations (conditional on availability of these new products in the public hospitals) would be to start patients on Zaltrap six-weekly, adding 50% more capacity, and then faricimab three-monthly, resulting in another 20% fewer injections. He also suggested that laser should be used more as a rescue remedy for diabetic macular oedema and branch retinal vein occlusion to target micro-aneurysms and exudates that develop, adding further cost savings.
Here’s hoping Dr Riley’s raised voice and persuasive arguments can be heard in the boardrooms of Te Whatu Ora and Pharmac.

Naomi Meltzer is an optometrist who runs an independent practice specialising in low-vision consultancy. She is a regular contributor to NZ Optics.