The challenge of assessing DED symptoms in children
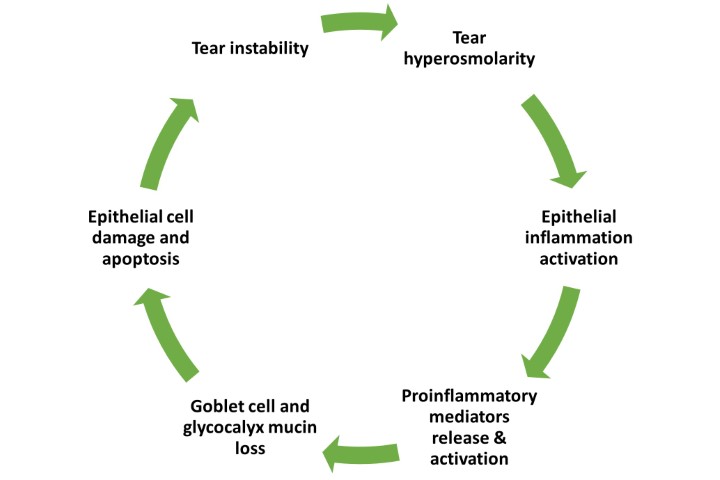
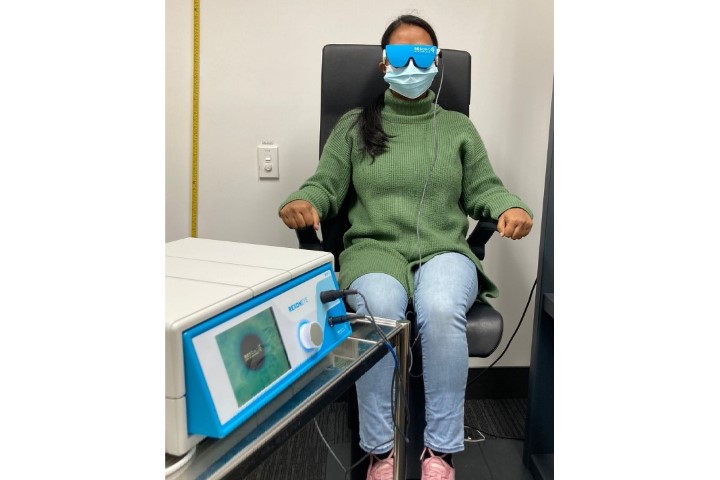
Detecting the presence and severity of dry eye (DED) symptoms is important in the diagnosis and management of ocular surface diseases1. With escalation in the use of digital devices and myopia control interventions in school-aged children, the measurement of ocular surface comfort has become of great relevance in the paediatric population2-4. To understand the impact of these environmental factors on the paediatric ocular surface health and quality of life, there is a need for reliable assessment of DED symptoms in children.
Symptom assessment challenges in children have been reported mainly in relation to chronic health conditions rather than eye conditions5. The unique challenges of using similar instruments to assess patient-reported outcomes in adults and in children are identified by the US Food and Drug Administration (FDA) and the European Medicines Agency. These include recognition of the lower age limit at which children can provide reliable and valid responses, vocabulary and health-concept comprehension6,7. A reliable measure of symptoms should be based on responses which come directly from the patient and are not dependent on interpretation by the clinician, investigator or parental carer6. Direct responses from patients are important for a thorough understanding of the disease impact and treatment effectiveness.
Assessing DED symptoms requires a validated questionnaire; however, none of the existing DED questionnaires have been validated for use in children1,8,9. Several clinical studies have attempted to measure DED symptoms in children aged 3-18 years using questionnaires developed for adults. These studies found this approach problematic as the questionnaires may adopt a format or contain concepts or questions that children do not understand or are irrelevant to them9. This may result in less effective data capture and potentially underreporting of DED symptoms in children.
The challenge of younger age
Research on cognitive paediatric processing capability of terms also commonly used in symptom questionnaires shows comprehension is low at five years old but increases from six years old, attaining maturation of logical reasoning similar to adults by the age of 1610.
Our recent study identified the challenges associated with the use of adult-validated DED questionnaires in children, showing those aged between 6-15 years vary in their ability to reliably complete them9. The study demonstrated existing DED questionnaires – including Ocular Surface Disease Index (OSDI), Symptoms Assessment in Dry Eye (SANDE), Numerical Rating Scale (NRS), Ocular Comfort Index (OCI), Dry Eye Questionnaire 5 (DEQ-5) and Instant Ocular Symptoms Survey (IOSS) – can be administered to children, but that younger children may need longer to complete them and assistance with some items.
Significantly more help was needed with specific questionnaire items and this was more often required by younger children, presumably due to difficulty understanding the meaning of some symptom descriptors (eg. grittiness, foreign-body sensation). We estimated the reading grade level of words in each questionnaire using the Flesch-Kincaid calculator, representing US grade levels of education. The OCI, DEQ-5 and IOSS are fairly easy, pitched at 6-7th grade reading level (ie. 11-13 years of age), the SANDE and OSDI are plain English at 8-9th grade reading level (age 13-15 years), while the NRS is fairly difficult at 10-12th grade reading level (15-18 years of age)9. These reading grade levels predict the likely level of assistance required for younger children.
Vocabulary and comprehension of concepts
Children who have very high vocabulary levels perform similarly to adults in terms of concept comprehension11, suggesting vocabulary may be more relevant than age in predicting the amount of assistance required for comprehension. Our study recommended use of DEQ-5 and IOSS questionnaires in paediatric patients, due to their relatively simple vocabulary and ease of use9.
In summary, development and validation of appropriate questionnaires for specific age groups is critical to accounting for age-related language comprehension difficulties and to determine the age limit at which reliable and valid responses can be obtained. Consideration could be given in future research to rewording specific items to be better understood by children, which may reduce the need for help during questionnaire administration. In the interim, practitioners can reliably use existing DED questionnaires by offering pre-scripted examiner assistance to children when needed.
References
1. Wolffsohn J, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. The Ocular Surface. 2017;15(3):539-574.
2. Chidi-Egboka N, Jalbert I, Golebiowski B. Smartphone gaming induces dry eye symptoms and reduces blinking in school-aged children. Eye. 2022:1-8.
3. Kim J, Wang M, Craig J. Exploring the Asian ethnic predisposition to dry eye disease in a pediatric population. The Ocular Surface. 2019;17(1):70-77.
4. Jaiswal S, Asper L, Long J, Lee A, Harrison K, Golebiowski B. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clinical and Experimental Optometry. 2019;102(5):463-477.
5. De Civita M, Regier D, Alamgir A, Anis A, FitzGerald M, Marra C. Evaluating health-related quality-of-life studies in paediatric populations: some conceptual, methodological and developmental considerations and recent applications. Pharmacoeconomics. 2005;23:659-685.
6. Food US, Drug A. Guidance for industry: patient-reported outcome measures: use in medical product development to support labeling claims. Fed Regist. 2009:65132.
7. Committee for Medicinal Products for Human U. European Medicines Agency. Reflection paper on the regulatory guidance for the use of health-related quality of life (HRQL) measures in the evaluation of medicinal products. July 27, 2005. In:2016.
8. Chidi-Egboka N, Briggs N, Jalbert I, Golebiowski B. The ocular surface in children: a review of current knowledge and meta-analysis of tear film stability and tear secretion in children. The Ocular Surface. 2019;17(1):28-39.
9. Chidi-Egboka N, Golebiowski B, Lee S-Y, Vi M, Jalbert I. Dry eye symptoms in children: can we reliably measure them? Ophthalmic and Physiological Optics. 2021;41(1):105-115.
10. Matza L, Patrick D, Riley A, et al. Pediatric patient-reported outcome instruments for research to support medical product labeling: report of the ISPOR PRO good research practices for the assessment of children and adolescents task force. Value in Health. 2013;16(4):461-479.
11. Borovsky A, Elman J, Fernald A. Knowing a lot for one’s age: vocabulary skill and not age is associated with anticipatory incremental sentence interpretation in children and adults. Journal of experimental child psychology. 2012;112(4):417-436.

Dr Ngozi Chidi-Egboka is a postdoctoral research associate at Save Sight Institute, University of Sydney, and a visiting fellow at the School of Optometry and Vision Science, UNSW Sydney, with specific research interest in cornea and ocular surface.

Associate Professor Blanka Golebiowski is based at UNSW Sydney’s School of Optometry and Vision Science. Her research aims to advance understanding of the mechanisms causing dry eye and eye pain with particular focus on blinking, digital screen time and corneal inflammatory response to contact lens wear.

Professor Isabelle Jalbert is deputy president of the Optometry Council of New South Wales and chair of the examination committee of the Optometry Council of Australia and New Zealand (OCANZ). Her research at UNSW Sydney focuses on evidence-based eyecare, eyecare quality and health education, with a parallel research focus on the links between the environment and the ocular surface.