Glaucoma research review
Virtual clinics for glaucoma care – patients’ and clinicians’ experiences and perceptions: a qualitative evaluation
Gunn J, Marks J, Au L, et al
Eye (2022) 36:209-218
Review: Virtual glaucoma clinics are being used throughout the world in an attempt to help address the increasing glaucoma burden facing clinicians within public hospital systems. This study specifically evaluated patient and clinician satisfaction from two virtual clinic setups in the UK.
Virtual clinics are where in-person doctor-patient interactions are replaced by two components. The first is a patient visit for clinical measurements including visual acuity, intraocular pressure, visual field, OCT and disc photography. Patient data collection is usually performed by a technician, nurse or optometrist. The second component is the reviewing of results by an ophthalmologist, nurse specialist or glaucoma-trained optometrist, and an outcome sent to the patient by letter. Specific criteria are usually set in place to determine patient suitability.
The authors found nearly 95% of patients had confidence and satisfaction in the person conducting the tests and most (>90%) were likely to recommend the service to family and friends. However, they also noted that 10% of patients were not happy to receive clinic results by post and 12% would have been happy to wait longer to see a doctor. There were also high levels of satisfaction reported among staff involved in the virtual clinic testing, as well as the clinicians involved in the reporting of results.
The authors concluded virtual glaucoma clinics can be acceptable to the majority of patients, staff and clinicians. Dissatisfaction was primarily related to poor communication rather than the service itself.
Comment: At Greenlane Clinical Centre we set up a rapid-imaging virtual clinic to manage overdue glaucoma follow-ups (visual acuity, intraocular pressure (IOP), ocular coherence tomography only), which have dramatically increased due to the pandemic. We are currently transitioning to full virtual clinics that include visual field testing. The rate-limiting step is primarily technician and clinic availability. It is reassuring to see the high level of patient and clinician satisfaction with virtual clinics in this study.
The Singapore asymptomatic narrow angles laser iridotomy study: five-year results of a randomised controlled trial
Baskaran M, Kumar R, Friedman D et al
Ophthalmology 2022;129:147-158
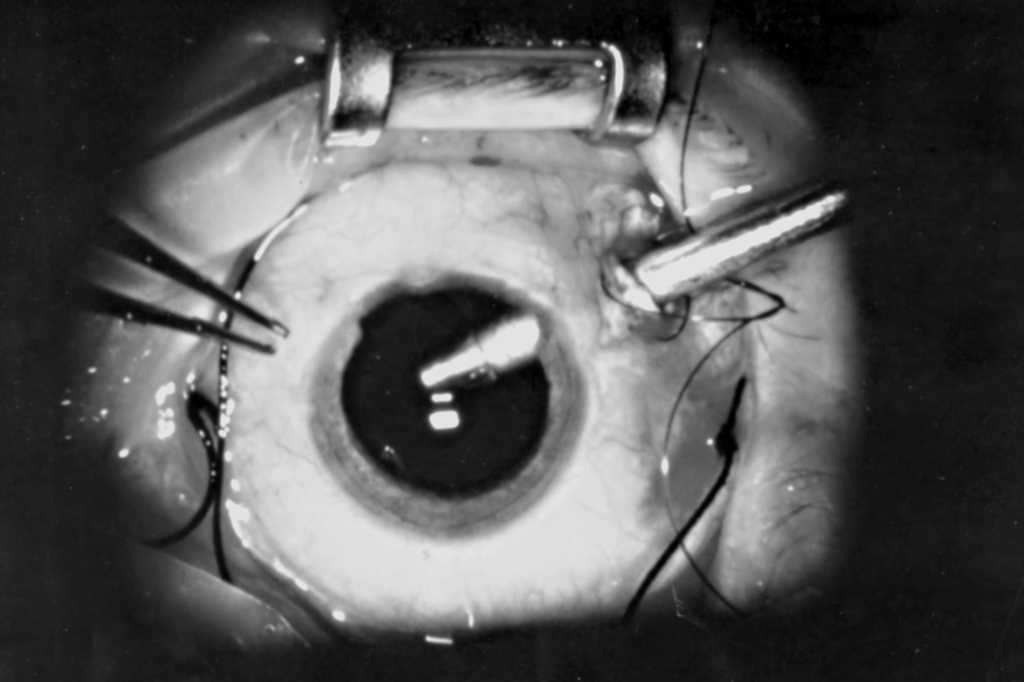
Review: The purpose of this study was to examine the efficacy of prophylactic laser peripheral iridectomy (LPI) in patients who received a primary angle closure suspect (PACS) diagnosis. Defined as 180° of iridotrabecular contact, PACS is generally benign but has been shown to progress to primary angle closure (PAC), acute angle closure (AAC) or primary angle-closure glaucoma (PACG) in some patients. Therefore, LPI has traditionally been recommended to treat PACS. This study examined the efficacy of LPI in patients with a PACS diagnosis.
Each participant underwent prophylactic LPI in one randomly selected eye; the fellow eye served as a control. Patients were followed up annually for five years. The primary outcome measure was development of PAC (defined as presence of peripheral anterior synechiae, IOP >21mmHg, or both or AAC or PACG over five years).
Of the 480 randomised participants, most were Chinese (92.7%) and were women (75.8%), with mean age of 63 years. The authors noted eyes not treated with LPI had twice the risk of PAC – the majority of which was the development of PAS only, rather than glaucoma. Older participants, particularly those with a higher baseline IOP, were more likely to develop PAC. However, they also noted the overall incidence of PAC or PACG was extremely low – 22 patients with LPI needed to be treated to prevent one developing PAC over a five-year timeframe.
Comment: These findings are consistent with those of the Zhongshan Angle Closure Prevention (ZAP) study and suggest observation without LPI is a reasonable option for PACS patients, unless they have specific high-risk factors, such as previous angle closure in the other eye, if they require frequent pupil dilation, if they have other glaucoma risk factors, or if they have symptoms consistent with angle closure (eg. episodes of eye pain, headache, and blurred vision).
Safety and effectiveness of the Preserflo MicroShunt in primary open-angle glaucoma: results from a two-year multicentre study
Beckers H, Aptel F, Webers C et al
Ophthalmology 2022; 129(5): 472-477
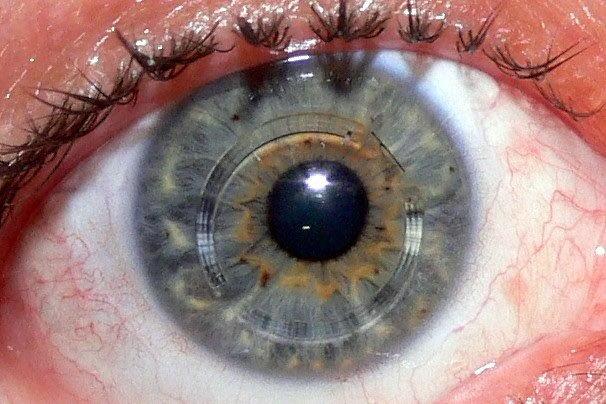
Review: The purpose of this study was to assess the safety and effectiveness of the Preserflo MicroShunt (formerly InnFocus MicroShunt) in primary open-angle glaucoma (POAG) patients.
Eligible patients (n=81) were aged 18-85 years with POAG inadequately controlled on maximal tolerated medical therapy with IOP ≥18 and ≤35mmHg or when glaucoma progression warranted surgery. Primary outcomes were IOP reduction and success at year one. Additional end points at year two included IOP reduction, success, glaucoma medications, adverse events (AEs) and reoperations.
Mean IOP decreased from 21mmHg at baseline to 14.5mmHg at year one and 14.1mmHg at year two. Overall success (with and without supplemental glaucoma medication) at year one and year two was 74.1%. Mean number of medications decreased from 2.1 at baseline to 0.5 at year two (p<0.0001), and 74% of patients with a successful outcome were completely medication free. Most common non-serious AEs were increased IOP requiring medication or selective laser trabeculoplasty (25.9%) and mild-to-moderate keratitis (11.1%). There were six (7.4%) reoperations and five (6.2%) needlings by year two.
That authors concluded mean IOP and glaucoma medication reductions were significant and sustained over two years post-surgery. No long-term, sight-threatening AEs were reported.
Comment: This device is increasingly being used by glaucoma specialists in New Zealand as an alternative to trabeculectomy surgery in suitable patients. The results of this study demonstrate promising one- and two-year results in terms of the overall success of surgery, reduction in medication use and safety profile.

Dr Hussain Patel is a cataract and glaucoma specialist at Eye Surgery Associates and Greenlane Clinical Centre in Auckland. He is also a senior lecturer with the Department of Ophthalmology, University of Auckland.