Medical retina research update
Efficacy, durability, and safety of intravitreal faricimab with extended dosing in patients with DMO
Wykoff CC et al
Lancet 2022; 399(10326): 741-755.
Review: Yosemite and Rhine are two phase 3 randomised, double-masked, non-inferiority trials conducted across 353 sites worldwide. A total of 1,891 patients with vision loss due to centre-involving diabetic macular oedema (DMO) were randomly assigned to intravitreal faricimab 6mg every eight weeks, faricimab 6mg on a personalised treatment interval (PTI) based on disease activity, or aflibercept 2mg every eight weeks.
At year one, both faricimab arms demonstrated non-inferiority to aflibercept for vision gains and improved anatomical outcomes. The safety profile was also comparable between the three treatment arms.
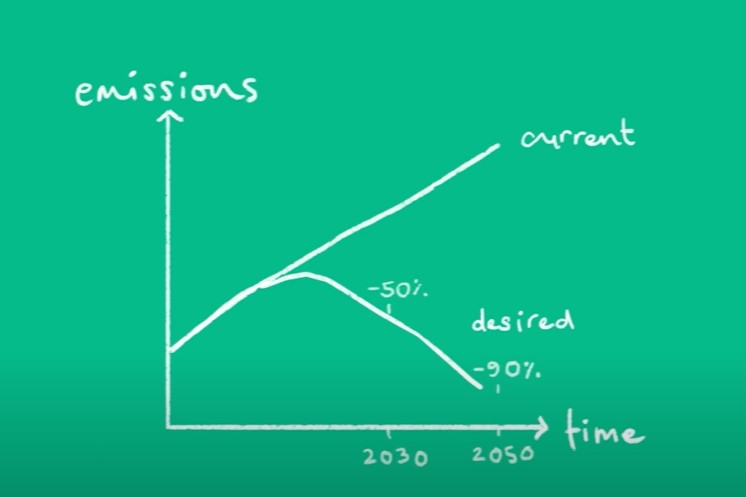
Comment: This study shows the efficacy of faricimab, a novel bispecific antibody, for improving vision and anatomical outcomes compared with aflibercept. That this was shown for adjustable dosing up to every 16 weeks, suggests there may be an advantage with dual Ang-2 and vascular endothelial growth factor (VEGF)-A pathway inhibition beyond VEGF pathway inhibition alone. Therefore faricimab may have potential for extended dosing intervals and a reduced treatment burden for patients with DMO.
Primary one-year results from similar studies (TENAYA and LUCERNE) looking at faricimab for neovascular age-related macular degeneration (AMD) also look promising. It will be worth looking out for the year-two results of these studies, which will be presented later in 2022, and long-term data when it becomes available.
Cataract surgery and the risk of developing late AMD: the age-related eye disease study 2, report number 27
Bhandari S et al
Ophthalmology 2022 Apr;129(4):414-420.
Review: This was a prospective cohort study within AREDS2 (Age-Related Eye Disease Study 2), the randomised controlled clinical trial of oral supplements for the treatment of AMD. The aim was to evaluate the risk of developing late AMD (geographic atrophy or neovascular AMD) after cataract surgery. It included AREDS2 participants aged 50-85 years with bilateral large drusen or unilateral late AMD with eyes that had not had cataract surgery and no late AMD at baseline. It compared those who then had cataract surgery and those who remained phakic for late AMD.
A total of 1,767 eligible eyes from 1,195 participants received cataract surgery, and 1,981 eyes from 1,524 participants developed late AMD. Patients were followed up for a mean of nine years.
Late AMD was identified in 408 eyes that received cataract surgery and in 429 phakic controls. Analysis did not show statistical difference between the two groups or increased risk of developing late AMD with cataract surgery.
Comment: According to this study, cataract surgery does not increase the risk of developing late AMD. This will be very reassuring for patients with macular degeneration and cataract. It provides a useful reference for discussing cataract surgery with and consenting these patients.
Archway randomised phase 3 trial of the port delivery system with ranibizumab for neovascular AMD
Holekamp NM et al
Ophthalmology 2022; 129: 295-307.
Review: This was a phase 3, open-label, randomised US trial evaluating the safety and efficacy of the port delivery system (PDS) with ranibizumab for treating neovascular AMD.
A total of 418 patients diagnosed within nine months of screening, previously treated with and responsive to anti-VEGF, were enrolled. They were randomised 3:2 to treatment with the PDS with ranibizumab 100mg/ml with fixed 24-week refill-exchanges or monthly intravitreal ranibizumab 0.5mg injections. Patients were monitored monthly. Those in the PDS arm could receive supplemental treatment with ranibizumab 0.5mg injection if disease activity was present.
The PDS arm showed non-inferiority and equivalence to the monthly ranibizumab arm and 98.4% did not receive supplemental ranibizumab treatment in the first 24-week interval. More ocular adverse events were reported in the PDS arm (19.0% vs 6.0%) and most of these were within the first month of implantation.
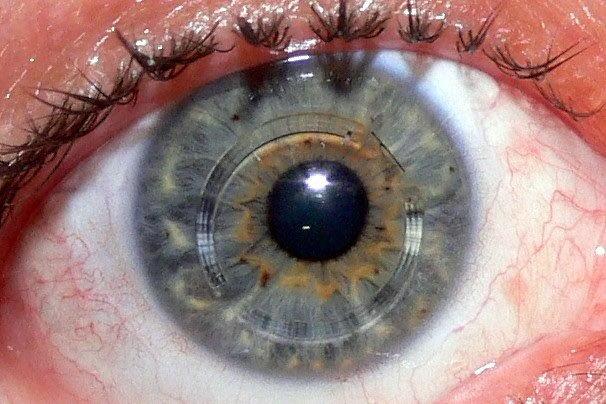
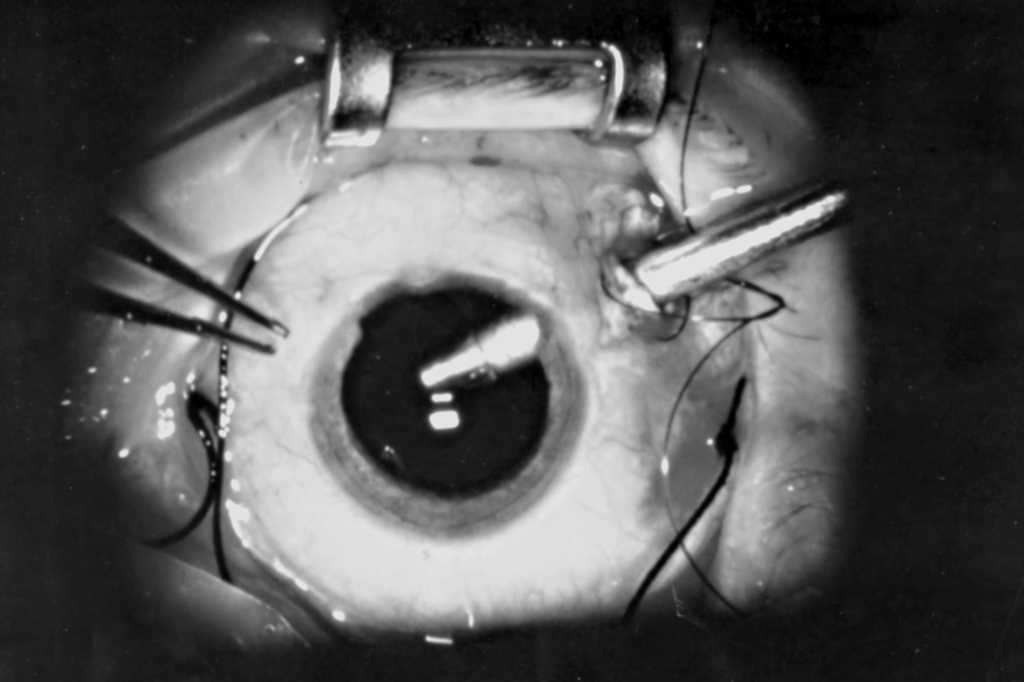
Comment: The port delivery system uses an permanent refillable implant inserted surgically in the operating theatre, with refill-exchanges done in clinic to deliver ranibizumab continuously into the vitreous for a sustained effect.
PDS has potential as a long-term treatment to reduce the treatment burden for neovascular AMD. It does carry risks associated with the surgical insertion, so more ocular adverse effects may occur. Further studies are required to confirm its effectiveness in patients with long-term disease on anti-VEGF treatment for longer, and longer follow-up data beyond 40 weeks is needed on the system’s performance and safety.

Dr Tracey Wong is a consultant ophthalmologist with subspecialist training in medical retina and visual electrophysiology. She is based in Auckland at Manukau Super Clinic and Greenlane Clinical Centre, and at Eye Surgery Associates.