There’s no vision like Snowvision
After a five-year hiatus and a shaky start due to inclement weather causing flight diversions and cancellations, Snowvision 2023 got underway with a traditional opening cocktail function in wintry Queenstown. Fortunately, the snow arrived just in time and by Thursday the bus to Coronet Peak was full of excited snow bunnies.
The conference followed the familiar format of early morning lectures and late afternoon seminars, with the middle of the day free for activities (or recovery, depending on the night before!). Long-serving sponsors Corneal Lens Corporation’s Graeme Curtis put on a fully subscribed clay skeet-shooting competition, while Glen Bolton from Independent Lens Specialists provided an equally popular golf day at Millbrook.


Long-serving Snowvision trustees Hamish Caithness and David Robinson
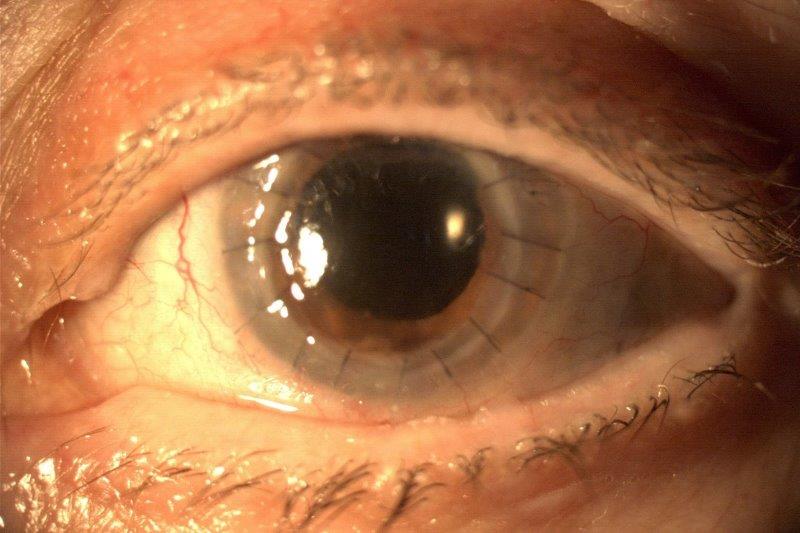
This year’s US-based guest speakers were Associate Clinical Professor Matt Bovenzi from SUNY, New York, and Professor Steve Ferruci from the Southern California College of Optometry in Los Angeles. Specialising in medical retina, Prof Ferruci walked us through the optimal management of age-related macular degeneration (AMD) and diabetic retinopathy (DR). He reminded us of the importance of the early detection of conversion from dry to wet AMD (such as recognising metamorphopsia) and discussed the use and efficacy of modern anti-VEGF agents and port-delivery systems. A newly FDA-approved C3 complement blocker, pegcetacoplan, is showing promise for interfering with the inflammatory cascade which causes geographic atrophy (GA) progression in the paramacular region. Prof Ferruci also reviewed what we should know about diabetes and eyes, explaining insulin resistance is strongly related to ethnicity and obesity, and the retinal outcomes are worse when overlapped with high blood pressure and high cholesterol. The haemoglobin A1c (HgbA1c) blood test result needs to be less than 7.0%, with 6-6.5% indicating pre-diabetes and a prompt to recommend weight loss, smoking cessation and more exercise. Symptoms of acquired type 2 diabetes include increased hunger, thirst and urination, weight loss, delayed wound healing, dry mouth, dry skin and refractive changes. DR is the leading cause of blindness in the 20-74-year-old age bracket, with type 1 patients having a high DR risk after 20 years, and up to 80% of people with type 2 developing DR after 15 years. With good blood sugar and blood pressure control, DR risk drops by about 35%. Prof Ferruci noted mild non-proliferative DR (NPDR) is characterised by peripheral microaneurisms/dot and blot haemorrhages, which can then worsen into cotton wool spots, indicating retinal ischaemia, while proliferative DR (PDR) is characterised by worse ischaemia triggering retinal neovascularisation and increased damage. Both NPDR and PDR can be treated with anti-VEGF injections, with NPDR also requiring laser photocoagulation, while OCT should be used to rule out diabetic macular oedema, he said.
Refer, relax or consider a crapsule?
Prof Ferruci’s final workshop, ‘Refer or relax retina’ provided excellent guidance on when to seek a second opinion. He covered lattice degeneration (usually watch with annual exams unless there is significant vitreous traction), horseshoe retinal tears (urgent referral for same-day laser), operculated holes (relax or refer, depending on size), retinoschisis (in diabetes, relax and review) and when to refer naevi and congenital hypertrophy of the retinal pigment epithelium. He shared a helpful mnemonic for this: TFSOM – thickness, fluid, symptoms, orange pigment, margins; thickness being the biggest risk, as melanomas are always more elevated. He also reviewed the signs and symptoms of a retinal detachment (RD) and advised a macular-on RD is a far more urgent referral.

Prof Steve Ferruci
Long-term Snowvision supporter and Auckland ophthalmologist Dr Trevor Gray gave two presentations, his first focused on gut dysbiosis and its association with certain eye conditions (see related story p16). He discussed how Westernised diets encourage bacterial gut imbalances, resulting in increased inflammation, vascular disease and immunocompromise, and are associated with greater risks of uveitis, AMD, glaucoma, DR and dry eye. He suggested we become more aware of methods of maintaining and restoring a balanced gut bacterial population, by using probiotics (live, good bacteria), prebiotics (food for good bacteria), faecal transplants (‘crapsules’ - which got a laugh) and promoting a healthy diet.
Dr Gray’s next workshop involved a guest appearance from his colleague Dr Simon Dean and some excellent advice on the management of dry eye. Dr Dean’s oculoplastic expertise helped us understand when it’s appropriate to make minor mechanical lid adjustments to improve tear flow and reduce evaporative dryness. Effective medications include tacrolimus ointment for vernal keratoconjunctivitis, oral azithromycin for meibomian gland disorder and fluorometholone or methylprednisolone for breaking the dry eye-blepharitis inflammatory cycle, he said. Among many other useful topics, Drs Dean and Gray also outlined scenarios for managing recurrent corneal erosions by minimising the shearing forces between the eyelids and corneal epithelium. Although radial keratotomy vision issues aren’t much helped by corneal crosslinking, pupil constriction agents, such as brimonidine and pilocarpine, may be visually helpful, they said.
Thinking like a GP
Now retired, the ever-popular Associate Professor Daryl Guest from the University of Melbourne returned to ask us to think about some eye problem scenarios as a GP would – to look at the patient’s overall situation before jumping to a diagnosis. For example, we should ask ourselves if a patient is generally well and are they likely to be medication-compliant? It’s also worth considering metabolic or systemic problems, checking bloods and blood pressure, he said, and if you’re unsure about the diagnosis, do a therapeutic trial with early follow up or seek a second opinion.
A/Prof Guest then teamed up with Greenlane Clinical Centre-based optometrist Richard Johnson to present a series of interesting cases. These included a 16-year-old’s bilateral papilloedema in reaction to minocycline for acne, a persistent corneal lesion not responding to antibiotics or antivirals (it was fungal), chlamydial keratoconjunctivitis and its implications, anterior uveitis secondary to poorly controlled type 2 diabetes and managing recurrent styes in a rural community with oral antibiotics and boiled saline. A/Prof Guest again suggested we try to think more like a GP (‘beware the unilateral red eye’) and gave us another mnemonic to help see the big picture: ISBAR – identify, situation, background, access-action, recommendation.
Five more interesting case studies were presented by Tauranga optometrist Alex Petty from his specialty contact lens practice: a rare and hard-to-treat fungal keratitis from a gardening accident; corneal trauma from a cracked ortho-k lens (always inspect at aftercares); a too-tight lens for keratoconus; utilising an oblate RoseK2 XL lens for postgraft; and some helpful ways of analysing axial length data and improving ortho-k lens designs to maximise myopia control (smaller treatment zone diameter and better return zone mould from a smaller back optic zone diameter design).
After Johnson’s always entertaining and embarrassingly difficult pathology quiz was won by Palmerston North’s Jacob Benefield, SUNY’s A/Prof Bovenzi reviewed some of the current and trending laser and minimally invasive glaucoma surgery (MIGS) treatments. Selective laser trabeculoplasty (SLT) is cost effective and becoming increasingly popular, often dropping IOPs by 15-30% while reducing the chances of nocturnal IOP spikes. It is contraindicated in narrow-angle, closed-angle and angle-recession glaucoma but can be very good for pigment dispersion, pseudoexfoliation and when there may be medication noncompliance or no effect. MIGS and iStent micro-tubes are proactive and increasingly popular treatments which can be included at the same time as cataract extraction and can reduce IOP by up to 40%, he said.
A/Prof Bovenzi went on to discuss the growing role of nutraceuticals in glaucoma, explaining the important essential vitamins and minerals for eye health and reminding us that head and body position (eg. yoga inversion, head position on side of pillow) can increase IOP. While there is a weak association with increased IOP and coffee consumption, antioxidant-packed foods such as green tea and saffron can have the opposite effect, possibly by keeping the trabecular meshwork unblocked. Ginkgo biloba and exercise may be neuroprotective, especially by helping ocular blood flow in normal-tension glaucoma; the tetrahydrocannabinol (THC) in cannabis, but not cannabidiol (CBD) oil, is also thought to lower IOP but only for a few hours; and an hour a day of deep breathing and meditation can lower IOP by up to 5mmHg in some people, said A/Prof Bovenzi. However, he cautioned that being largely unregulated, the nutraceutical industry suffers from relatively weak scientific study evidence.

Prof Jennifer Craig and Renata Watene
The nerves of some people!
A/Prof Bovenzi’s final seminar was entitled ‘You have some nerve! Optic disc oedema differential diagnosis and management.’ He broke the topic down into ischaemia, axoplasmic transport and inflammation. OCT imaging can be very useful to look at the thicknesses of the neuroretinal rim and the retinal nerve fibre layer, both of which can be increased in optic nerve swelling. The ganglion cells can initially cope with this, but if sustained over more than three months it can develop into optic nerve atrophy. Important diagnostic tests include vision, pupil testing, colour vision/red cap desaturation, OCT, erythrocyte sedimentation rate and C-reactive protein blood tests.
A/Prof Bovenzi then gave an overview of arteritic and non-arteritic anterior ischaemic optic neuropathy (AION). Giant cell arteritis (GCA) is an ocular emergency; symptoms include scalp tenderness and jaw claudication. The less serious non-arteritic AION is associated with diabetes, hypertension and hypercholesterolemia causing lowered circulation to the optic disc. Bilateral papilloedema can be caused by either serious compressive disorders raising the intracranial pressure (ICP), such as an intracranial meningioma (often associated with headaches and seizures – check pupil function for afferent defect) or Graves disease (hyperthyroidism). Benign idiopathic intracranial hypertension is most commonly associated with obesity in middle-aged females but can also be induced by medications that cross the blood-brain barrier, such as the acne treatment isotretinoin. Other symptoms of raised ICP include headache, tinnitus, transient visual obscuration and sometimes diplopia from sixth cranial nerve compression. Absence of spontaneous venous pulsation is another clue prompting investigations including MRI and a lumbar puncture to measure the cerebrospinal fluid pressure. Inflammatory optic neuritis is unilateral and often associated with pain on eye movement and indicates early multiple sclerosis (blood tests are antinuclear antibody and angiotensin converting enzyme); visual contrast sensitivity can also be reduced. A/Prof Bovenzi concluded by mentioning two masquerader conditions: pseudopapilloedema (small, crowded optic nerves in hyperopes) and optic disc drusen, which can often be seen on an OCT scan.
By day three a bit of fatigue had set in, so Dunedin ophthalmologist Dr Logan Mitchell’s amusing delivery of some cranial nerve palsies cases and adult strabismus was very welcome. He quickly covered the signs and symptoms of a sixth cranial nerve (abducens with a long pathway) palsy causing lateral rectus weakness and sudden esotropia, how checking the optic nerve for venous pulsation can discount an anomaly in ICP – IOP and central retinal venous pressure should be similar to each other – and how saccades can help ascertain myogenic or neurogenic cause. Differential diagnoses include compression from raised ICP, trauma, a microvascular ischaemic event (most common), inflammation or infection, or congenital. Such cases often resolve spontaneously over several months and can be managed by either monocular occlusion or a temporary Fresnel prism.
Dr Mitchell also touched on what to watch out for in Bell’s palsy and nerves three and four palsies – N4 palsies with a small hypertropia are usually longstanding with a tell-tale head posture and not sinister. Acquired adult strabismus can have a wide spectrum of causes from harmless decompensation of a childhood strabismus (and often previous surgery) or cranial nerve palsies to serious disease such as a brain tumour. He reminded us when operating on adult strabismus (for cosmesis or psychosocial reasons) only two extraocular muscles can be manipulated at one time and outcomes can still be variable.
The conference concluded with an excellent dinner at the newly refurbished Skyline gondola restaurant. Snowvision scholarship trustee Hamish Caithness thanked the attendees, speakers, sponsors and co-organisers for another fun event and announced the next three scholarship winners, Luke Oliver from Wellington, Jason Shen from Hamilton and Carmen Liu from Auckland (see related story).
Snowvision’s trustees are now looking for a new conference committee. Enquiries from energetic volunteers should go to hcaithness@xtra.co.nz.
Grant Watters is a therapeutically qualified optometrist specialising in specialty contact lenses, and a director of Mortimer Hirst in Auckland. He is also an honorary academic in both the School of Optometry and Vision Science and the Department of Ophthalmology at The University of Auckland.
Pictures courtesy of Dr Simon Dean.