Case study: Steroids and strimmers
Eye injuries from line trimmers (also known as strimmers, weed eaters, weed whackers and brush cutters) result from high velocity foreign body impact, causing mechanical tissue disruption and microbial contamination with bacteria and fungi¹.
In traumatic infective keratitis, it is necessary to remove microorganisms (clean and debride) and limit anatomical damage (repair)². Topical corticosteroids are believed to suppress inflammation caused by the infection, therefore decreasing pain or discomfort, and reduce corneal scarring, theoretically improving visual outcomes. However, this risks exacerbating the infection itself due to localised immunosuppression³. Here we report two line trimmer corneal injury cases treated with topical corticosteroids that developed fulminant infective keratitis.
Case reports
A 29-year-old Caucasian male presented with a one-day history of right eye pain, redness, photophobia and visual loss. He denied contact lens wear or recent trauma. Best corrected visual acuity (BCVA) was 6/9.5 right and 6/6 left eye. Examination revealed conjunctival injection, a 0.1mm paracentral corneal epithelial defect, anterior stromal opacity, fine keratic precipitates and 2+ anterior chamber cells. Dilated exam demonstrated no posterior segment inflammation. Right acute anterior uveitis with a corneal scar was diagnosed. Hourly topical prednisolone acetate 1% drops with four times daily chloramphenicol 0.5% drops cover were commenced.
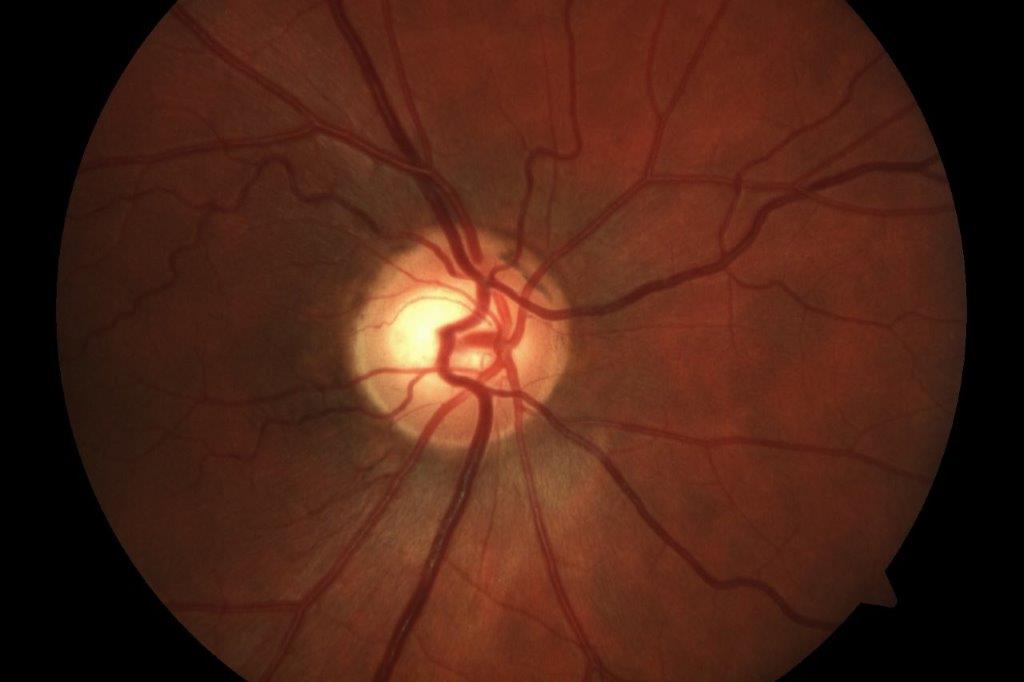
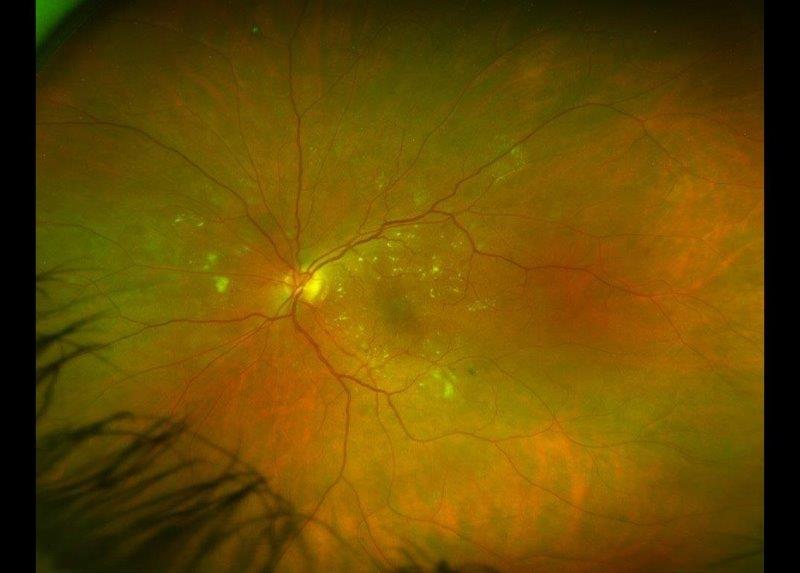
Four days later, the patient’s eye pain and visual loss worsened. He now reported using a line trimmer the day before but did not recall experiencing injury. The corneal ulcer and stromal opacity appeared larger. The diagnosis was revised to traumatic microbial keratitis and the prednisolone drops stopped. Intensive cefuroxime 5%, tobramycin 2% and natamycin 5% drops, as well as oral moxifloxacin 400mg daily, doxycycline 100mg bd and ascorbic acid 1g tds were started. Corneal scrape grew Streptococcus pneumoniae, but no fungi. Herpes simplex virus and acanthamoeba PCR were negative. Despite vigorous treatment, corneal thinning and hypopyon developed, before slow gradual improvement. Over three months, antibiotic drops were tapered, resulting in a final BCVA of 6/7.6 with a paracentral corneal scar and troublesome glare (Fig 1).

Fig 1. Bacterial keratitis, three weeks post line trimmer-related injury
The second case involved a 60-year-old Caucasian lady presenting with left eye pain and blurred vision after being hit by a stone from a line trimmer operated by another person. BCVA was 6/5 right eye, 6/6 left and slit-lamp exam showed a partial thickness corneal laceration, debris under the corneal flap and macrohyphaema, but no corneal infiltrate. Primary corneal repair was performed and neomycin-polymyxin B-dexamethasone drops were started.
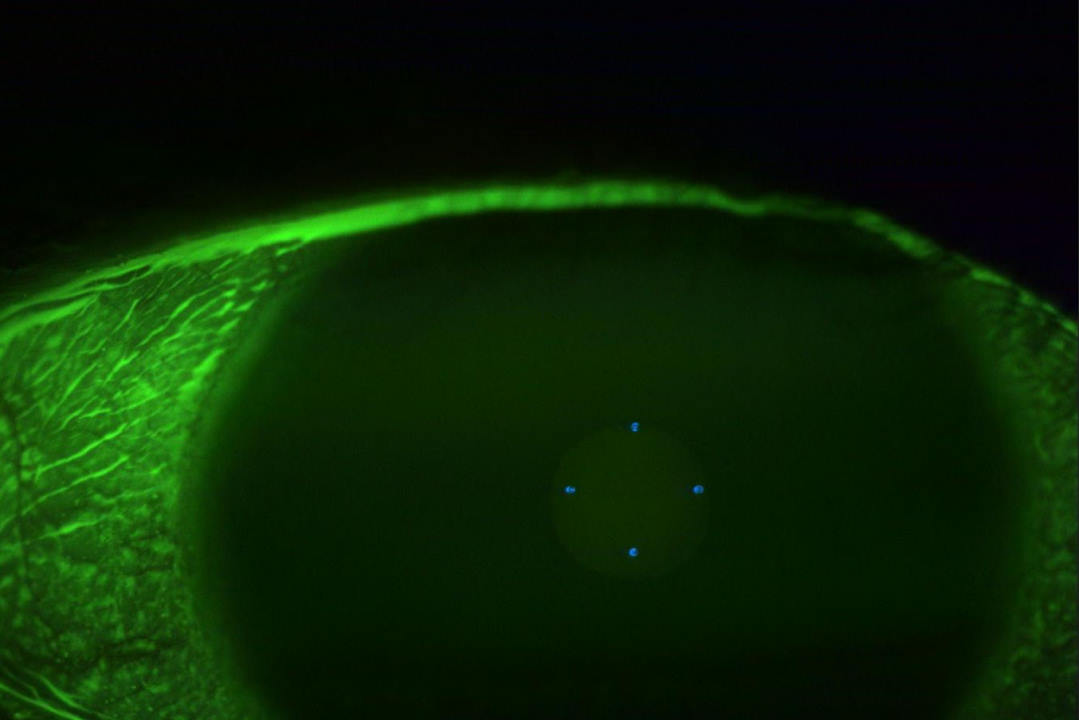
Two weeks later, she returned with increasing pain and visual loss. Examination demonstrated a new corneal epithelial defect, infiltrate and hypopyon (Fig 2). A corneal scrape showed hyphae and the culture grew scanty fungus and Nocardia nova complex. Acanthamoeba PCR was negative. Despite intensive topical and oral treatment with antibiotics and antifungals, no progress was noted. Tectonic penetrating keratoplasty was performed but graft failure ensued, with phthisis and subsequent enucleation of that eye one year later.

Fig. 2. Nocardia-fungal keratitis, one month post line trimmer-related injury
Discussion
The role of topical corticosteroids as a treatment adjunct in bacterial keratitis is debatable and it is contraindicated in fungal keratitis³’⁴’⁵. Although current evidence does not suggest significant harm or benefit from using topical corticosteroids in bacterial keratitis (only when used as an adjunct to topical antibiotics), usually after one to two days of antibiotic treatment, the authors believe the utmost caution should be paid when topical corticosteroids are used in contaminated corneal injuries, given the risk of bacterial and fungal keratitis.
There is particular evidence that patients with Nocardia keratitis who received topical corticosteroids fared worse than those who did not⁴’⁵. Care must be taken to rule out or identify an infective cause. The judicious use topical corticosteroids in such cases, needs to be given under the close observation of an eye specialist following a period of stability and/or improvement with appropriate antibiotic and/or antifungal cover.
We thank the patients for their consent to publish this case report.
References
- Taneja M, Ashar JN, Mathur A, Nalamada S, Garg P. Microbial keratitis following vegetative matter injury. Int Ophthalmol. 2013;33(2):117-23
- Stern GA, Buttross M. Use of corticosteroids in combination with antimicrobial drugs in the treatment of infectious corneal disease. Ophthalmol. 1991;98(6):847-53
- Palioura S, Henry CR, Amescua G, Alfonso EC. Role of steroids in the treatment of bacterial keratitis. Clin Ophthalmol. 2016;10:179-86
- Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, Glidden DV, et al. Corticosteroids for Bacterial Keratitis: The Steroids for Corneal Ulcers Trial (SCUT). JAMA Ophthalmol. 2012;130(2):143-50
- Ni N, Srinivasan M, McLeod SD, Acharya NR, Lietman TM, Rose-Nussbaumer J. Use of adjunctive topical corticosteroids in bacterial keratitis. Curr Opin Ophthalmol. 2016;27(4):353–357
Dr Kelvin Ngan is a non-training ophthalmology registrar with Nelson Marlborough District Health Board serving Nelson and Wairau Hospitals, with prior ophthalmic experience in Wellington and Hawkes Bay.
Dr Sacha Moore is a consultant ophthalmologist with the Nelson Marlborough District Health Board, specialising in cornea and anterior segment surgery.