Eye and mitey: dealing to Demodex with ivermectin
Demodex species form part of our natural microflora but in certain conditions can overpopulate, causing recurrent and persistent blepharitis and meibomian gland dysfunction (MGD). Since Soolantra 1% (ivermectin) cream has been successfully used off-label overseas for several years in the treatment of Demodex blepharitis, we wanted to see if we could replicate these results in New Zealand. Our Soolantra study at Wellington’s Thorndon Eye Clinic began in October 2023 and is ongoing, with three-to-six-month reviews.
Introduction
Demodex folliculum live in the upper part of hair follicles (eyelids/lashes, nose, cheeks, chin, scalp and ear), while Demodex brevis can live all over the body but is typically found in chest and neck areas. At just 0.15-0.4mm long, both species are relatives of ticks, spiders and scorpions and live in hair follicles and sebaceous glands (the meibomian glands, in the case of blepharitis). Their scales and a palpus – a seven-clawed organ that grabs cells – help them to remain in place; they also possess a chelicera – a retractable needle that sucks out the contents of our cells1-3. Up to six mites can inhabit one eyelash follicle, causing dislocation and loss of the lash.
Creatures of the night, they emerge from the follicle as we sleep to eat dead skin cells and excess oils. Then they mate on our eyelids, lashes and face, returning to the follicles to lay their eggs. They become adults within one week and live for two. When they die, their dead cells and excreted toxins cause irritation and lead to blepharitis and MGD2,3. Patients will complain of itch, redness, epiphora, crusty discharge, stinging and loss of eyelashes. Children under five years, those aged 20-30 years and the elderly and immunocompromised are most susceptible to infection.
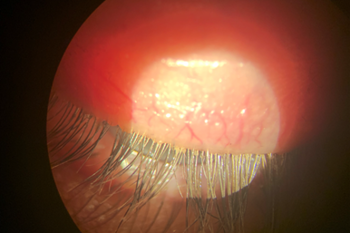
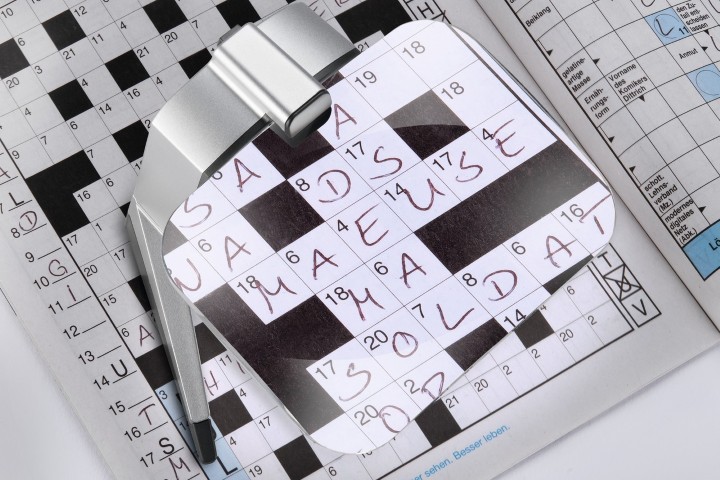
Fig 2. Collarettes and debris on eyelash base
In New Zealand, Soolantra 1% (ivermectin) cream is classified as an S29 antiparasitic and anti-inflammatory medicine for the treatment of rosacea. First used in 1971 in oral form to deworm animals, it has been used to treat human intestinal parasites since 19866,7. Ivermectin invades Demodex’s Ca2+ channels, increasing cell permeability and causing their contents to leak. This ‘flaccid paralysis’ is the source of the mild irritation felt by some people. Although known as a temporary side effect (characterised by red, inflamed eyes and eyelids) and occurring in less than 1% of patients in the literature, our study had an incidence of 4% (n=2).
Our study subjects were the first 50 patients with demodicosis (raised numbers of Demodex causing Demodex blepharitis) we encountered in our clinic. The patients ranged from 18-91 years, with 40 females and 10 males.
Method
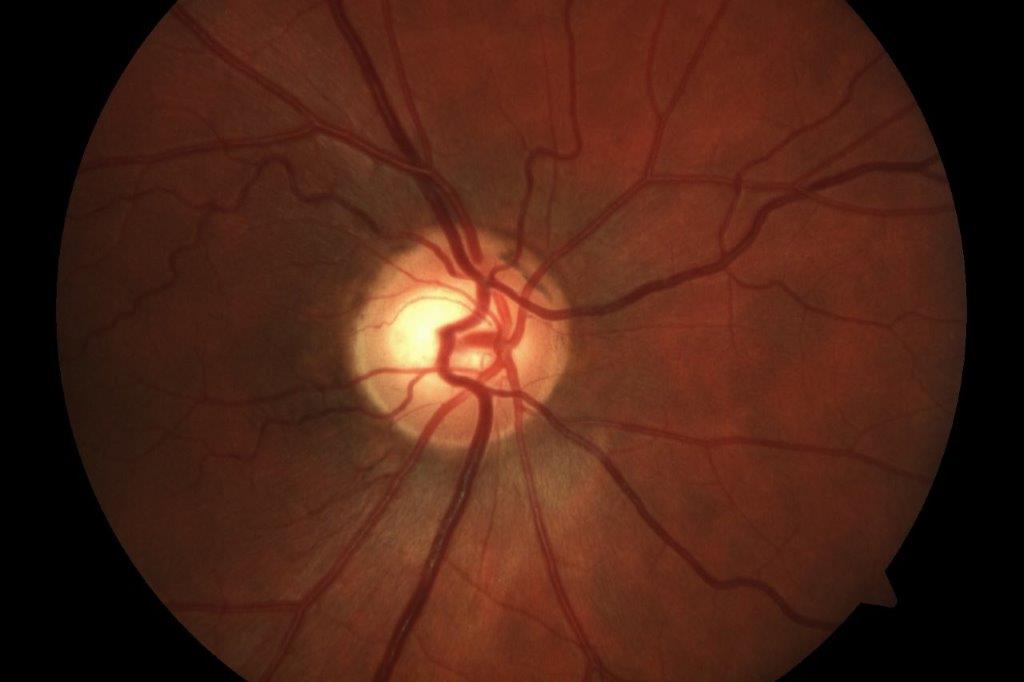
Based on Dr Craig Helm’s 2022 paper, ‘Treatment of ocular Demodex infestation with topical ivermectin cream’1, our study identifiers were pouting (Fig 1), debris, collarettes (Figs 2 and 3) and patient symptoms. At review, only clinical signs were considered (percentage improvement).
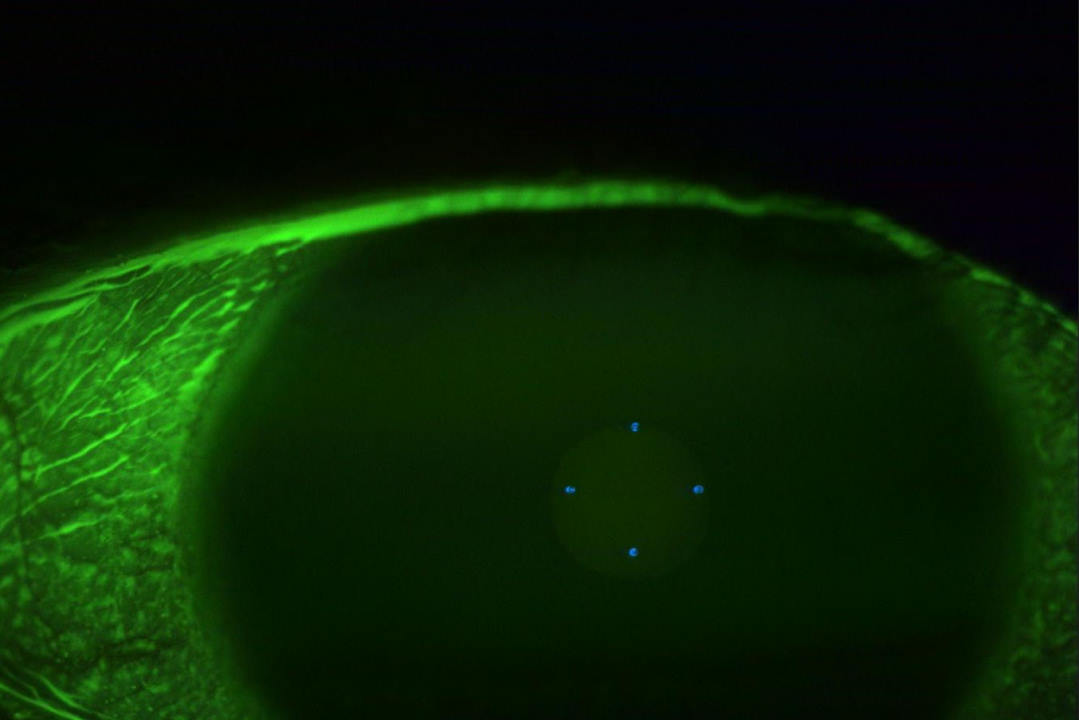
Soolantra 1% cream was applied to upper and lower eyelids with a cotton bud with the patient’s eyes closed (Fig 4). After 10 minutes, the cream was removed using a sterile saline flush, followed by wiping of the inner superior and inferior lid margins with more cotton buds until no clumps of cream remained. If required, one drop of saline was applied to flush any remnants on the ocular surface.
Following first application, reviews were completed at two-to-four weeks, four-to-six weeks and three-to-six months. At the two-to-four week review a second application was offered, even if no significant Demodex (NSD) – defined as less than 5% pouting, collarettes or debris – was seen. Some patients declined. However, where there was less than 95% improvement, we recommended retreatment, due to Demodex’s two-week lifecycle. The same criteria were applied to the four-to-six week and three-to-six-month reviews.
Results
- After one Soolantra application, 80% of patients (n= 40) had greater than 80% removal, with 20% (n=10) of them showing NSD. All patients made this initial first review (see Fig 6)
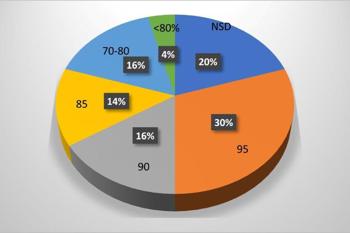
Fig 6. After first treatment. Outer numbers indicate % of symptom resolution; inner
(grey box) numbers indicate % of patients
- After two Soolantra applications, 90% (n=36) of the remaining patients achieved >90% removal, of which 67.5% (n= 27) achieved NSD. One patient exited; one did not attend (DNA). 10 patients did not have a second treatment (see Fig 7)
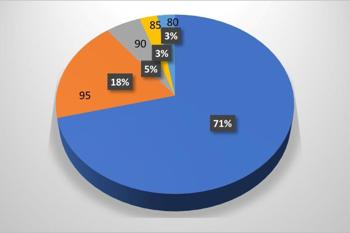
Fig 7. After second treatment
- Nine patients received three Soolantra applications, with all achieving >95% removal (NSD). Three DNA (see Fig 8)
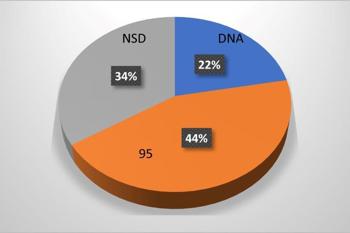
Fig 8. After third treatment
- After 3-6 month follow-up (ongoing), 74% (n=23) achieved NSD and 26% have required further Soolantra application (n=8). There are 17 more patients to be seen, with one DNA and one who exited the study
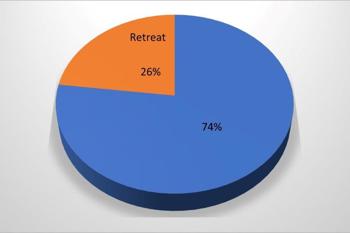
Fig 9. At 3-6 month review (ongoing)
Taking a closer look at reinfection rates at 3-6 month (ongoing) review, of the patients who only had one initial Soolantra treatment, none developed further demodicosis (n=5); of those requiring two initial treatments, 89% required no further Soolantra, with only 11% requiring further application (n=18); and of those patients requiring three initial treatments, 14% required no further Soolantra while 86% required further application (n=7).
Discussion
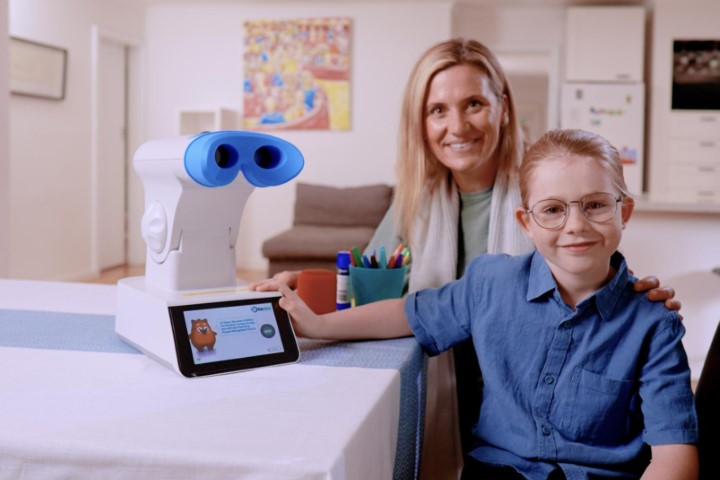
When considering why reinfection occurs, although many factors could be at play, we observed it was predominantly patients with rosacea who were affected (Fig 5). Rosacea was seen at all ages in our study. Of rosacea’s four variations, the ones we most commonly see is the facial blush – erythematotelangiectatic – and ocular.
It is known that skin areas with rosacea have increased numbers of Demodex mites. However, it is unknown if rosacea increases the number of mites, if the increased number of mites causes rosacea, or whether the bacteria living on the mites (Staphylococcus and Bacillus oleronius) are responsible2,8.
Our elderly patients and those immunosuppressed suffered reinfection, probably due to them having less resilience to commensal microbes that easily repopulate. Patients with giant papillary conjunctivitis and/or contact lens wear also faced reinfection. Possibly this was due to them touching their eyes more, leading to increased spread.
Heavy makeup on eyelids and lashes also allowed Demodex to re-establish, while makeup containers may be a good breeding ground for young Demodex. Poor facial and linen hygiene can also readily re-establish demodicosis. Since Demodex can live away from the human host for hours to days3, advice includes washing bed linen, pillowcases and towels at least weekly. Use the hottest wash available, consider using bleach and use the hot cycle in your dryer, even after air drying. Also consider a new pillow4. Discard opened eye makeup and remove false lashes and face and eye makeup really well. Clean the eyes and face twice a day with a dedicated warm flannel and put it in the laundry at the end of the day.
Conclusions
Soolantra 1% (ivermectin) cream is extremely effective in decreasing Demodex load on human eyelids and lashes. It can be effective on some people after a single treatment and we have shown the condition can be managed for up to six months. We will continue to use it in our clinic on existing and future patients.
References
- Scanes, C 2018, Animals and Human Society in Sciencedirect.com
- Fischer, K 2023. What are Demodex Mites?, webmd.com
- McBain A, et al 2016. Science direct.com
- Najafi-Tagol, K, 2003. New approaches for fighting demodex mites. www.news.medical.net/health/(title).aspx
- Am J Ophthalmol Case Rep. 2022 Jun; 26: 101551. Treatment of ocular Demodex infestation with topical ivermectin cream. Published online 2022 Apr 21. PMCID: PMC9058595PMID: 35509284
- www.ncbi.nim.nib.gov. PMC10507222 (topic: Ivermectin) and PMC4807898
- www.drugs.com
- Webmd.com ‘Acne rosacea’ search
Frances Misich is a clinical optometrist at Thorndon Eye Clinic, Wellington, with particular interests in dry eye and glaucoma.