GNZ Symposium: exploring every angle
On a rare, sunny winter Sunday, it seemed a shame to head indoors for Glaucoma New Zealand’s (GNZ’s) sixth symposium but, as always, it was a rewarding day which delivered excellent learning and networking opportunities across the professions.
Glaucoma specialist Dr Ridia Lim talked to us (via Zoom) from Australia, describing the metabolic rabbit hole she has been down in pursuit of novel ways to arrest chronic disease. She questioned whether glaucoma is another insulin-related disease – diabetes type 4? – and proposed a case where the root cause of glaucoma, mitochondrial dysfunction, leads to oxidative stress and neuroinflammation. Describing the disordered energy metabolism and the role of insulin in neurodegeneration, she asked if we focused more on what not to eat, rather than on what supplement to take, could a keto (low-carb) diet play a role in treating glaucoma through improved metabolic health? It was a provocative start to the day, ending with the fact that using fat for energy, as opposed to glucose, also burns less B3, a vitamin being considered an adjunct therapy for glaucoma.
Dr Sam Kain, together with GNZ chair Professor Helen Danesh-Meyer, hosted this year’s symposium sessions, featuring punchy 10-minute presentations in the morning, followed by talks with an interactive component after lunch.
Keeping it simple
Dr Hussain Patel provided some sage advice about visual fields, reminding us that while they’re a vital tool in glaucoma diagnosis and management, normal fields do not signify a lack of glaucoma. Included in his pragmatic checklist was the learning curve, considering artefacts in the results, the trigger-happy patient and the presence of other pathology and myopia.
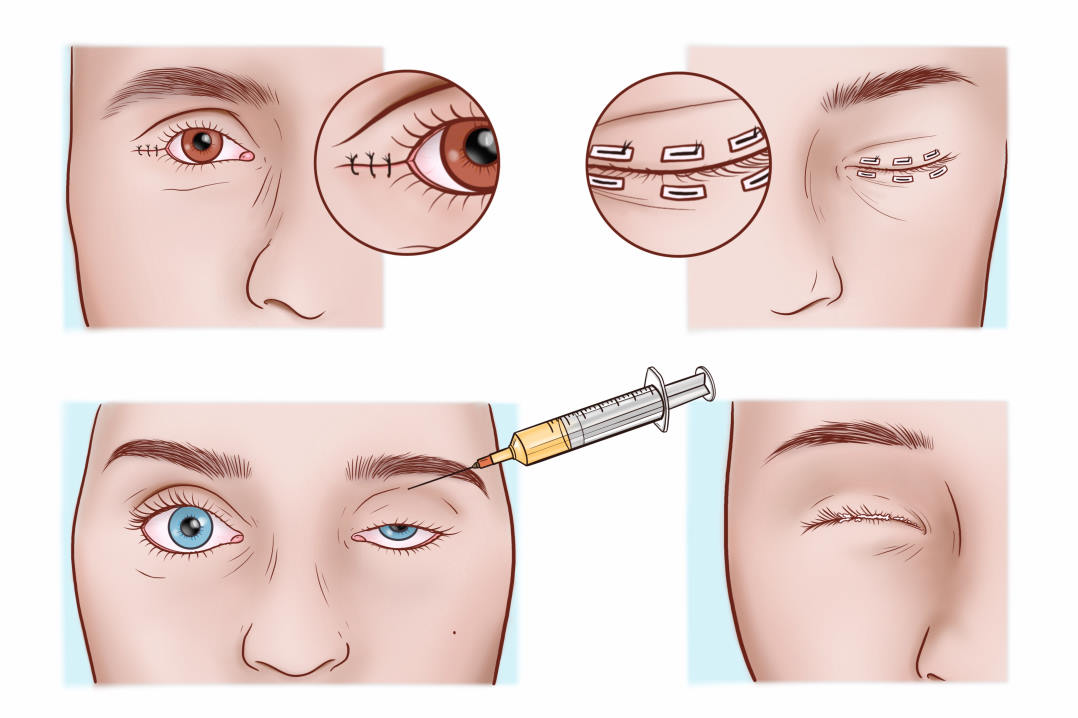
Dr Divya Perumal then offered some tips on managing narrow angles. Alongside reminders of the risk factors (ethnicity, gender, ocular anatomy and refractive error), she offered a ‘SImPle’ almost-acronym for gonioscopy: structure, iridocorneal touch, plateau iris and pigment. She also directed us to use the GNZ fact sheets in patient education, in particular the acute angle closure and peripheral laser iridotomy ones when referring patients for an ophthalmology assessment. Later in the day Dr Perumal described her process of preparing patients for future selective laser trabeculoplasty (SLT) by simply walking them past the laser in clinic. Helpful and practical – such gems occur regularly during these symposiums!
Dr Jesse Gale presented two topics in person this year, the first on OCT in glaucoma. Again packed with practical tips on how we can use our growing cache of data to detect glaucoma, he discussed ‘red, green and in between’. It’s tricky to identify early, evolving glaucoma when analysis puts measurements in the ‘green zone’, he said, while suggesting we look at the ‘time’ measurements when we have ‘red’ disease.
Normal tension glaucoma (NTG) was next on Dr Gale’s agenda. A thoughtful approach, once you’ve ruled out non-glaucomatous optic neuropathy, is to consider if this is glaucoma, then why, he said. Has the IOP been high in the past, are there contributing lifestyle factors or vascular factors at play? He certainly succeeded in his stated aim of not presenting boring talks!
Entitled ‘Clinical markers of glaucoma progression’, Dr Shenton Chew reminded us of the goal to maintain quality of life by balancing disability prevention with the burden of treatment. So, if increased IOP is not a marker of true progression, how do we assess the stability of the structural and functional nerve? He encouraged us to take the time to understand and explore our OCT data, looking for more subtle indicators, such as identifying which disc zone is showing most change.
The panel discussions at the close of each session also gave us a number of small pearls, one example being, “The fundamental idea is that the past is a predictor of future; so if the past findings are stable, we rely on the fact they will remain stable.”
Smarter than the average bear
When to treat and when to monitor ocular hypertension (OHT) was a topic presented by Dr Graham Reeves. While useful reminders from the Ocular Hypertension Treatment Study (OHTS) can guide our decisions on when to treat OHT, as healthcare professionals our aim is to maintain or improve the health of our patients, which should be balanced with the psychological effect of chronic disease, he said. Dr Reeves then quoted a delightful Yosemite park ranger, who said, “There is considerable overlap between the intelligence of the smartest bears and the dumbest tourists.” The challenge is to find the sweet spot, or, in Yosemite terms, the optimum garbage-can design, to apply when we have an asymptomatic condition (OHT), which is a major and treatable risk factor for a blinding eye condition.
Dr Rahul Dwivedi began his presentation with a disclaimer, admitting he loves SLT. He referenced the Light study, which compared SLT to drop treatment, and referred to the National Centre for Health and Care Excellence in the UK, which lists SLT as a first-line treatment. Arriving at Canterbury DHB, Dr Dwivedi set out to compare the trial findings to his real-world situation. He found SLT use was haphazard and varied across clinics. Subsequently, he wrote clear guidelines and trained registrars, including in SLT use, for cases of pigmentary and pseudoexfoliative glaucoma.
Optometrists Dr Hannah Kersten, Inhae Park and Richard Johnson presented interesting glaucoma cases for discussion. These included Dr Kersten’s update on how multifocal pattern electroretinogram (ERG) may be useful but has yet to be established as a routine tool.
The day closed with research updates from this year’s Gordon Sanderson Scholarship recipients. Studying communication in glaucoma, Esther Kim described how we can use tools to improve this in practice, including the ‘ask-tell-ask’ approach, which begins with asking patients what they understand about their condition. Meanwhile, fellow scholar Daniel Zhang has been deep diving into the UK Biobank and its 1,000 MRI scans of glaucoma patients, so we hope to hear more on this in due course. Among the many pearls that popped up, I was reminded that in 2022 Dr Kersten proposed that the best time to treat glaucoma is prior to ganglion cell apoptosis – before vision loss. This year, Prof Danesh-Meyer spoke of the commitment point, when ganglion cells are going to die, no matter what.
Overall, it was once again a thoroughly worthwhile day, which I recommend adding to your 2024 CPD calendar.
Claire McDonald is an optometrist working in private practice in Warkworth. In 2017 she completed the University of Auckland (UoA) advanced glaucoma care credentialing course, supervised by Dr Hussain Patel. Until recently, she worked part time with ADHB glaucoma patients in the UoA clinic.