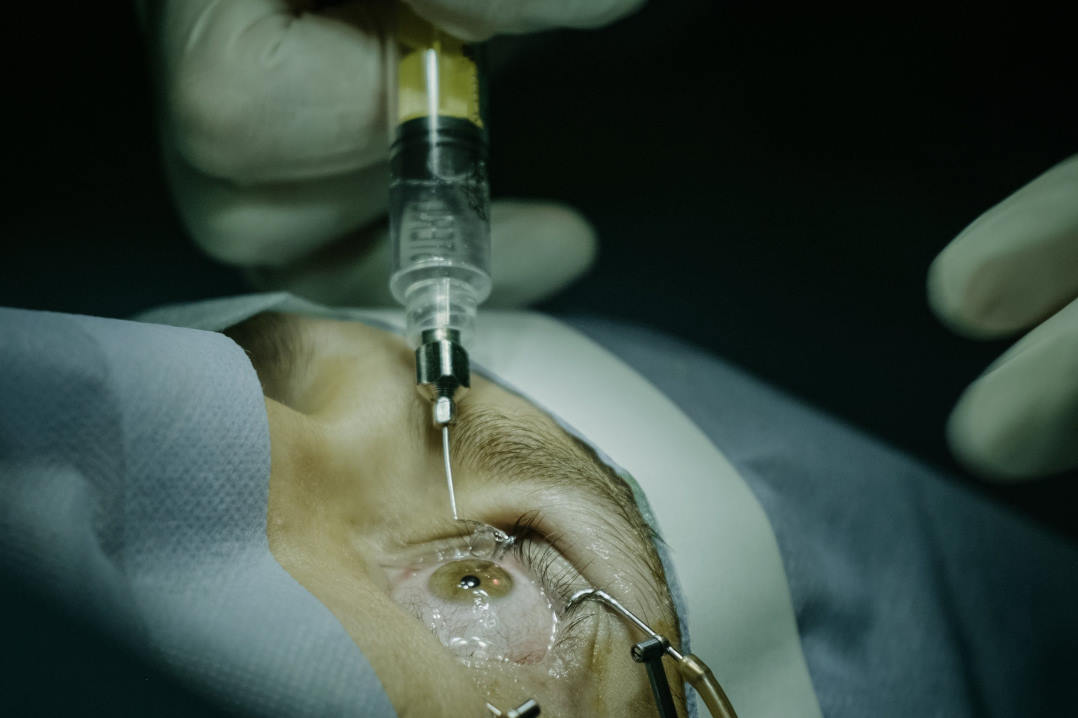
Human model to test cataract implant surgery
Researchers at the University of East Anglia in collaboration with Hoya Surgical Optics have improved a laboratory model that simulates cataract surgery on human donor eyes, allowing evaluation of artificial intraocular lens (IOL) implants under conditions that better reflect the post-surgical environment.
During cataract surgery, the eye’s cloudy natural lens is removed and replaced with an IOL. Initially, outcomes from cataract surgery are superb, but a haziness known as posterior capsule opacification (PCO) can develop in a significant number of patients following surgery.
At the moment the only treatment for PCO is laser surgery - which is expensive and not without risks. There is therefore a need to better understand the physiological events driving PCO and to better manage the condition.
The human capsular bag model was pioneered at UEA in the 1990s and has progressively evolved with time.
Lead researcher Professor Michael Wormstone, from UEA’s School of Biological Sciences, said: “Our model now mimics the transient nature of inflammation that patients experience after cataract surgery. It is more reflective of clinical events and allows comparative evaluation of different types of IOLs.”
The team used this clinically relevant model to assess the influence of two commercial IOLs (Alcon Acrysof and Hoya Vivinex) on PCO management.
Their findings showed that cell growth on the posterior capsule was reduced, light-scatter in the central visual axis was found to be lower and growth on the IOL surface was significantly reduced with the Hoya Vivinex IOL relative to the Alcon Acrysof and concluded “our model system predicts that the Hoya Vivinex is better able to manage events leading to PCO than the Alcon Acrysof IOL”.
The research was funded by Hoya Surgical Optics and The Humane Research Trust.