Lifestyle and stress linked to DED
The Auckland Dry Eye Epidemiology Study is a large population-based, multi-arm, cross-sectional study based at the Ocular Surface Laboratory (OSL) at the University of Auckland. It aims to characterise modifiable and non-modifiable risk factors of dry eye disease (DED) and address some of the gaps in the existing DED epidemiology literature identified by the 2017 global consensus TFOS DEWS II reports. Recently, two further sub-studies of the Auckland Dry Eye Epidemiology Study have been published in peer-reviewed journals1,2.
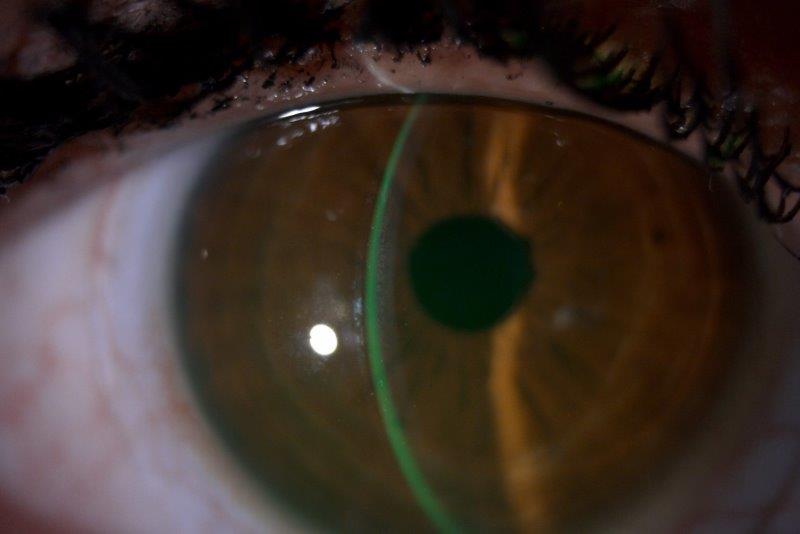
The first study investigated modifiable lifestyle factors of dry eye disease in a cohort of 322 healthy community residents with no previous history of major systemic or mental health conditions1. Overall, 34% of participants in this cohort had a positive diagnosis of dry eye disease according to the global consensus TFOS DEWS II criteria. Multivariate regression analysis demonstrated that advancing age, female sex, East Asian ethnicity and increased digital screen exposure time were positive risk factors for DED, while a higher level of caffeine consumption was a protective factor.
The association between digital screen exposure time and DED is consistent with the trends identified in the Royal Society Summer Science Exhibition Dry Eye Study3. The protective effect of caffeine was in agreement with earlier prospective crossover studies, which report the stimulation of increased aqueous tear production following caffeine consumption, although the underlying mechanisms are not fully understood4.
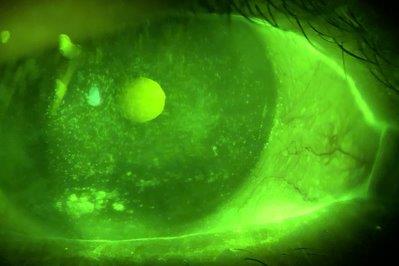
The second study evaluated the relationship between DED subtypes, psychological stress burden and self-perceived health status in a separate cohort of healthy community residents with no previous history of major systemic or mental health conditions2. Overall, 35% of participants fulfilled the global consensus TFOS DEWS II criteria for dry eye disease. Aqueous deficient DED was present in 10% of participants and evaporative dry eye disease in 31%. Multivariate analysis demonstrated a positive association between increased psychological stress burden and both DED subtypes. In addition, higher levels of self-perceived health status correlated with decreased odds of both aqueous deficient and evaporative DED. The study findings demonstrate the wide-reaching impact of dry eye disease and highlight the need for optimised management.
References
- Wang MTM, Muntz A, Mamidi B, Wolffsohn JS, Craig JP. Modifiable lifestyle risk factors for dry eye disease. Cont Lens Anterior Eye. 2021 (in press), doi: 10.1016/j.clae.2021.01.004.
- Wang MTM, Muntz A, Wolffsohn JS, Craig JP. Association between dry eye disease, self-perceived health status, and self-reported psychological stress burden. Clin Exp Optom. 2021 (in press), doi: 10.1080/08164622.2021.1887580.
- Wolffsohn JS, Wang MTM, Vidal-Rohr M, et al. Demographic and lifestyle risk factors of dry eye disease subtypes: A cross-sectional study. Ocul Surf. 2021;21:58-63.
- Osei KA, Ovenseri-Ogbomo G, Kyei S, Ntodie M. The effect of caffeine on tear secretion. Optom Vis Sci. 2014;91(2):171-7.

Dr Michael Wang is a neuro-ophthalmology clinical research fellow and a PhD student in the Department of Ophthalmology at the University of Auckland.