Lifestyle costs to our ocular surface
“Flight NZ29 is ready to board at Gate 4…” I’m in transit in Houston Airport, returning from my first in-person attendance in four years at the Association for Research in Vision and Ophthalmology conference (ARVO). As I mentally prepare for the 14.5 hours aboard my waka rererangi, I reflect on what a blast the last week has been – conference attendance was great, the poster halls were buzzing and the science was fabulous. Networking opportunities abounded and between each fascinating session, breakfast, lunch, dinner meetings and coffee catch-ups with colleagues offered windows to exchange ideas while sampling the culinary delights of the Deep South. Inevitably, there were some late nights, many early mornings, a cocktail here or there… it’s a lifestyle to be envied in many ways, but we have to wonder, does this come at a price in terms of the impact on our health and, specifically, our ocular surface health?
The topic is at the forefront of my mind as I stand, armed with my laptop and a to-do list longer than my arm, meticulously planning my plane time, which will involve staring at my digital screen without interruption, or much sleep, in a low-relative-humidity environment. Each of these risk factors individually – let alone in combination – can threaten ocular surface and tear film homeostasis. Plus, I’m a contact lens wearer, who regularly wears eye makeup!
A huge undertaking
Increasing awareness and understanding of ocular surface impacts from the lifestyle choices we make and the challenges we face can provide an opportunity for us and our patients to reconsider some choices and adopt mitigation strategies to help minimise impacts. This was the concept behind the Tear Film and Ocular Surface Society’s (TFOS’) decision to focus on ‘lifestyle’ for its latest international workshop, which I had the privilege of chairing.
It’s exciting to see the evidence-based reports arising from this TFOS Workshop – ‘A Lifestyle Epidemic: Ocular Surface Disease’ – now being published in peer-reviewed literature as a special issue in The Ocular Surface. Review of the relevant literature has been a mammoth task; one which required the input of 158 ocular surface clinical and academic experts from 38 countries, including four members from New Zealand: myself (chair) and Drs Kalika Bandamwar (contact lenses), Stuti Misra (nutrition) and Alex Müntz (digital environment). Citing thousands of references that were scrutinised and evaluated for their level of evidence, it’s no wonder the process has taken over two and half years. I’ve been honoured to be part of the leadership team that also includes Associate Professor David Sullivan as workshop organiser, vice-chair Professor Monica Alves from Brazil and Amy Gallant Sullivan, TFOS executive director, co-founder and fundraiser. TFOS is also grateful to the wide range of industry sponsors who provided unrestricted funds to support the workshop.
A steering committee was appointed and subcommittees were formed to address eight topic areas (highlighted below), encompassing relevant aspects of modern life which contribute to the development or exacerbation of ocular surface disease¹. To further strengthen the evidence-based nature of the workshops, an evidence quality subcommittee was established to offer guidance on the evidence quality assessment of the narrative reviews across all topic area reports and lead a systematic review answering a key clinical question as part of each report².
Unveiling the results
The focus of each topic report was how lifestyle choices impact the health of the ocular surface, recognising we make a variety of decisions every day that can have direct or indirect effects on our ocular surface health.
- The Lifestyle Challenges subcommittee determined that social, mental and physical factors all play a role in the development of dry eye disease³. In addition, sleep disorders, obesity, migraine, chronic pain syndrome, fibromyalgia and sleep apnoea have been associated with ocular surface disorders
- The Cosmetics subcommittee showed the constituents of cosmetics worn around the eye can be a direct risk factor for ocular surface disorders, so individuals should exercise caution when selecting eye makeup products⁴
- The Contact Lens subcommittee reiterated that contact lens (CL) wear, a well-known risk factor for dry eye disease, can be a rewarding and liberating experience as long as appropriate lifestyle choices are made⁵. It also suggested that with increased convenience, better compliance and fewer side effects, daily disposable CLs are a superior choice over reusable CLs
- The Societal Challenges subcommittee demonstrated how various factors can potentially impact both systemic and ocular health. Evidence suggests exercise, recreational drug use, hobbies, traditional medicines, domestic violence, mental and physical health, access to healthcare and eyecare, and socioeconomic status can contribute, though the need for more high-quality evidence was acknowledged⁶
- The Nutrition subcommittee highlighted that what we eat influences our ocular surface health⁷. They suggested looking beyond simply treating the ocular surface to collaborating with dietitians to investigate and better manage the root causes of ocular surface disease, particularly in cases of severe dry eye associated with nutritional deficiencies. A holistic approach that considers both dietary factors and ocular health may improve practitioners’ abilities to better identify and address underlying causes of ocular surface disease, ultimately promoting better health outcomes for patients
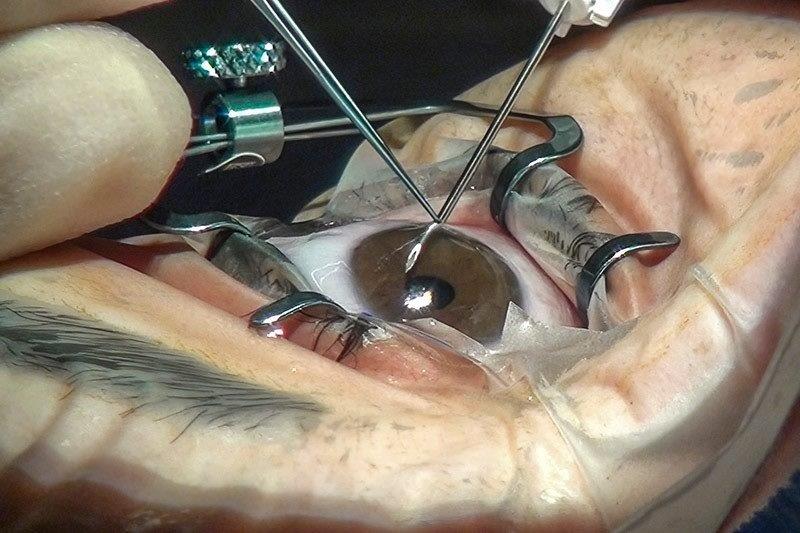
- The use of non-prescribed, over-the-counter medications is widespread and uptake of elective surgical procedures is more common than ever before. Based on published evidence, the Elective Medications and Procedures subcommittee warned that such interventions have the potential to adversely impact ocular surface health⁸. Increasing awareness of the potential risks, benefits and consequences was identified as key to helping patients make appropriate decisions when considering these options
- The Environmental Challenges subcommittee recognised that indoor and outdoor environments could pose direct and indirect threats to the ocular surface. Exposure to ultraviolet radiation and allergens risk development or exacerbation of conditions such as pterygium and allergic conjunctivitis, respectively. The impact of air, water and soil pollution were identified as areas that need further evaluation for their impact on ocular surface health. Increased awareness of possible challenges can help patients mitigate impacts from potentially modifiable risk factors⁹
- With reliance on computers, tablets and smartphones, screen use has become ubiquitous in everyday life. The Digital Environment subcommittee noted that average screen viewing hours are increasing and prolonged digital viewing is a risk factor for digital eye strain¹⁰. Improving blinking, optimising the work environment and encouraging regular breaks may help to improve ocular surface health. Contrary to popular belief, current evidence suggests blue-light blocking interventions are not an effective management strategy for digital eye strain
The TFOS Lifestyle Workshop reports have not only compiled and summarised existing scientific evidence but have also highlighted areas that require further research. Identifying gaps in the literature is vital to ensuring we provide evidence-based recommendations for our patients managing ocular surface health concerns. Conference presentations and professional articles will be forthcoming, but in the meantime, with the published reports being made freely available online (www.tearfilm.org), you’re encouraged to take a look!
References
- Craig J, Alves M, Wolffsohn J, Downie L, Efron N, Galor A, et al. TFOS Lifestyle: Introduction. Ocul Surf. 2023 (in press).
- Downie L, Britten-Jones A, Hogg R, Jalbert I, Li T, Lingham G, et al. TFOS Lifestyle - Evidence Quality Report: Advancing the evaluation and synthesis of research evidence. Ocul Surf. 2023 (in press).
- Galor A, Britten-Jones A, Feng Y, Ferrari G, Goldblum D, Gupta P, et al. TFOS Lifestyle: Impact of lifestyle challenges on the ocular surface. Ocul Surf. 2023 (in press).
- Sullivan D, da Costa A, Del Duca E, Doll T, Grupcheva C, Lazreg S, et al. TFOS Lifestyle: Impact of cosmetics on the ocular surface. Ocul Surf. 2023 (in press).
- Jones L, Efron N, Bandamwar K, Barnett M, Jacobs D, Jalbert I, et al. TFOS Lifestyle: Impact of contact lenses on the ocular surface. Ocul Surf. 2023 (in press).
- Stapleton F, Abad J, Barabino S, Burnett A, Iyer G, Lekhanont K, et al. TFOS Lifestyle: Impact of societal challenges on the ocular surface. Ocul Surf. 2023 (in press).
- Markoulli M, Ahmad S, Arcot J, Arita R, Benitez-del-Castillo J, Caffery B, et al. TFOS Lifestyle: Impact of nutrition on the ocular surface. Ocul Surf. 2023 (in press).
- Gomes J, Azar D, Baudouin C, Bitton E, Chen W, Hafezi F, et al. TFOS Lifestyle: Impact of elective medications and procedures on the ocular surface. Ocul Surf. 2023 (in press).
- Alves M, Asbell P, Dogru M, Giannaccare G, Grau A, Gregory D, et al. TFOS Lifestyle: Impact of environmental conditions on the ocular surface. Ocul Surf. 2023 (in press).
- Wolffsohn J, Lingham G, Downie L, Huntjens B, Inomata T, Jivraj S, et al. TFOS Lifestyle: Impact of the digital environment on the ocular surface. Ocul Surf. 2023 (in press).

Professor Jennifer Craig is chair of the TFOS workshop, ‘A Lifestyle Epidemic: Ocular Surface Disease’ and head of the Ocular Surface Laboratory (OSL) at the University of Auckland’s Department of Ophthalmology. She was vice-chair of TFOS DEWS II.
Prof Craig would also like to acknowledge the support and involvement of OSL research fellow Dr Kalika Bandamwar in collating this report.