Risks of topical ocular antibiotics and corticosteroids
The use of corticosteroids in ophthalmology was first introduced in the 1950s by Gordon and McLean1. Corticosteroids exert their anti-inflammatory effects via the inhibition of arachidonic acid and its eicosanoids (prostacyclins, prostaglandins, thromboxanes and leukotrienes). Topical corticosteroids play a paramount role in the management of a variety of inflammatory ocular conditions including uncomplicated anterior uveitis, control of post-surgical inflammation, prophylaxis and corneal allograft rejection treatment, stromal and endothelial herpes simplex keratitis, as per the Herpetic Eye Disease Study (HEDS), and occasionally aspects of keratoconjunctivitis sicca1.
Corticosteroid adverse events
The use of ophthalmic corticosteroids is well-known to be associated with a number of adverse effects, most notably the formation of cataract, raised intraocular pressure (IOP) with potential development of glaucomatous optic neuropathy, and exacerbation or reactivation of viral keratitis. The effect on IOP appears to be dose-dependent, while susceptibility to a pressure response may be attributed to genetic differences and variations in corticosteroid receptors1. Formulations that include more viscous composition or micro-suspensions increase ocular contact time and may double the steroid concentration in the cornea and aqueous humour compared with the same drug given as a solution2.
The systemic effects of topically applied ocular corticosteroids are generally agreed to be virtually negligible. Roters3 reported a statistically significant reduction in plasma cortisol that remained within physiological range in 13 postoperative cataract patients given hourly dexamethasone 0.1% eye drops for three days. Howes4 demonstrated undetectable loteprednol etabonate levels with normal plasma cortisol levels in 14 volunteers randomised to a regime of loteprednol 0.5% eye drops for 42 days.
Combination antibiotic-corticosteroid preparations
An acute red eye is a common ophthalmic presentation and is a cardinal sign of ocular inflammation. Fortunately, most cases are relatively benign with no overt ocular sequelae. With the advent of combination preparations containing topical antibiotics and corticosteroids such as Maxitrol (dexamethasone, neomycin, and polymyxin B), there may be some who favour this combined (anti-inflammatory, anti-infective) ‘blanket’ treatment for red eye management. The enthusiasm for such combined preparations has been attributed to the simplicity of allowing patients to administer fewer drops postoperatively, thereby improving patient compliance and lowering patients’ out-of-pocket costs.
Limitations of antibiotic-corticosteroid preparations
However, the use of combination therapy without a clear indication, or when the distinction between infective and inflammatory aetiologies is uncertain, may potentially culminate in microbial infection exacerbation, reactivation of latent herpetic infection, secondary infections, exposure to adverse steroid effects and development of antibiotic resistance. A New Zealand study investigating the risk factors of severe infective keratitis reported approximately 25% of patients admitted with microbial keratitis had recently received topical corticosteroids5.
The choice of an antibiotic is based on considerations of pharmacokinetic, pharmacodynamic and bacteriological characteristics. Neomycin is a bactericidal aminoglycoside antibiotic that is isolated from Streptomyces fradiae. While it has good coverage against several clinically important gram-positive and gram-negative organisms, including Staphylococcus aureus, Escherichia coli, Haemophilus influenzae, Klebsiella spp, and Proteus spp, there is inadequate activity against streptococci and no coverage for Pseudomonas aeruginosa and anaerobes – key pathogens in ocular infections. Therefore, to broaden coverage and reduce the emergence of resistant strains, neomycin is virtually always used in combination with other topical antibiotics, and Polymycin B is frequently added to cover Pseudomonas spp.
Common side effects of topical neomycin include hypersensitivity, irritation, stinging, burning and, in systemic use, a risk of auditory and vestibular ototoxicity in patients with renal or hepatic failure6. Notably, topical neomycin has been implicated as the aminoglycoside with the most significant deleterious effect on corneal epithelial cell function and frequent exposure results in more inflammatory cytokines and matrix metalloproteinase with subsequent corneal melting7. Cross resistance with framycetin has also been reported, while microbiological resistance is fairly common6.
Assessing antibiotic resistance
Antibiotic resistance is a mounting problem within ophthalmology. The crisis of antimicrobial resistance has been ascribed to antibiotic-prescribing practices including widespread and inappropriate use of broad-spectrum antibiotics for systemic infections, and there have been clarion calls for their use to be curtailed. The difficulty with studying antibiotic resistance against topical antibiotics used in ophthalmology is the effects may not be directly analogous to antibiotic resistance when compared with systemic use. Topical antibiotics can obtain extremely high concentrations compared with their systemic counterparts, so even when an antibiotic may be considered resistant, it may still be effective at killing bacteria, given the high levels of antibiotic in the ocular tissue.
All susceptibility and resistance data are derived using Clinical and Laboratory Standards Institute (CLSI) procedures based on systemic treatment breakpoints from serum and plasma levels of antibiotics, so they may not correspond to topical or intravitreal treatments – hence the need to scrape and culture microbial keratitis to confirm the organism and determine sensitivity and resistance. Fortunately, the opportunity for bacterial resistance to spread from patient to patient is limited in ophthalmology. Conditions such as endophthalmitis, keratitis and blepharitis are not associated with bacterial spread, and the self-limitation of conjunctivitis may not allow sufficient time for antibiotic resistance to develop.

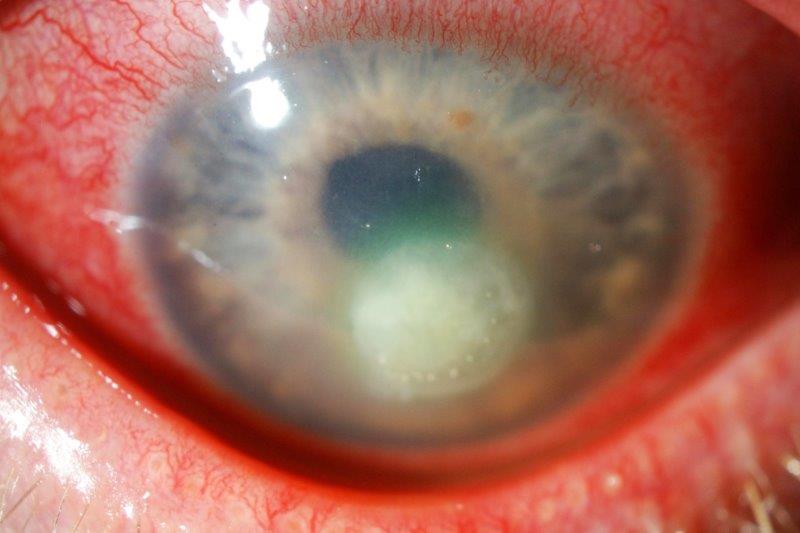
Fig 2. A 55-year old female with blepharitis-related staphylococcal ulcer with delayed healing and ciprofloxacin deposits within the corneal epithelial defect due to prolonged use of topical ciprofloxacin with preservatives
Trends in fluroquinolone and chloramphenicol resistance
Studies of antibiotic susceptibility in normal ocular flora have demonstrated 10-20% resistance to second and third-generation fluoroquinolones8. Fourth-generation fluoroquinolones, such as moxifloxacin, were developed to combat Pseudomonas aeruginosa infections resistant to second-generation fluoroquinolones, but there are increasing reports of fourth-generation fluoroquinolone-resistant keratitis8.
Currently, the rate of antibiotic resistance in New Zealand is relatively low compared with other countries. A study in Waikato reported 99% sensitivity to ciprofloxacin in bacterial organisms isolated from 265 corneal scrapes9. While eyecare professionals have no control over the use of systemic fluoroquinolones, national guidelines have been implemented to limit unnecessary antibiotic use. Notably, the emphasis on antimicrobial stewardship which promotes judicious use of antibiotics, including conversion from intravenous to oral antibiotic use, batching of intravenous antimicrobials, therapeutic substitutions and formulary restriction. Appropriate consultation with infectious disease specialists also helps to encourage heterogeneity through individualisation of drug selection.
Interestingly, recent studies of antibiotic resistance in the UK and Australia demonstrated that microbes isolated from cases of bacterial keratitis are just as susceptible to chloramphenicol when compared with fluoroquinolones, especially in cases of methicillin-resistant Staphylococcus aureus – although chloramphenicol is not generally recommended in the treatment of microbial keratitis. Similar findings were reflected in local research, including a Wellington study that reported chloramphenicol sensitivity in all gram-negative and gram-positive isolates from 34 corneal scrapes10 and a Christchurch study, which demonstrated chloramphenicol sensitivity in 89% of gram-negative isolates and all gram-positive isolates from 87 corneal scrapes11.
Ongoing role of chloramphenicol in ocular infection
Chloramphenicol is a bacteriostatic antibiotic produced by Streptomyces venezuelae and introduced in 1948. It is widely used to treat bacterial conjunctivitis and for post-operative prophylaxis but its bacteriostatic nature and lack of efficacy in Pseudomonas aeruginosa infection make it unsuitable for treating bacterial keratitis. Nonetheless, topical chloramphenicol possesses a reasonably broad spectrum of activity and is highly effective against gram-positive and gram-negative organisms as well as most anaerobes. With high differential solubility resulting in high intraocular penetration, chloramphenicol is superior to most other antibiotics for prophylaxis in ocular surgery6. Topical chloramphenicol is generally well tolerated with uncommon adverse effects of hypersensitivity and transient stinging2.
Chloramphenicol and blood dyscrasias
There have been historical concerns regarding the association between chloramphenicol and aplastic anaemia following a study by Wallerstein12 in 1969 that reported the incidence of chloramphenicol-induced aplastic anaemia (from systemic use) was 13 times that of the idiopathic form. Similarly, Fraunfelder13 published a case report in 1982 and cited three other cases of fatal aplastic anaemia associated with topical chloramphenicol. Citing these studies, Doona and Walsh14 argued that topical chloramphenicol should not be used as a first-line treatment of bacterial conjunctivitis in the UK and erroneously suggested fusidic acid and framycetin as equally effective options for treating most superficial ocular infections. While fusidic acid primarily targets gram-positive organisms, framycetin has limited bacterial sensitivities to Staphylococcus aureus and gram-negative organisms6. Acquired resistance has also been reported for both of these antibiotics6. The association between topical chloramphenicol and aplastic anaemia was also refuted in later studies, with previously cited cases noted as poorly documented, with some patients found to be taking other medications associated with blood dyscrasias6,15. Using high-performance liquid chromatography, Walker measured serum chloramphenicol levels of patients who were given chloramphenicol eye drops four times daily for 1-2 weeks15. Samples taken four hours after their last doses did not demonstrate a detectable level of chloramphenicol in the serum, making it difficult to justify the possibility that chloramphenicol or its metabolites reached a sufficiently high level to cause blood dyscrasias in the dose-related manner documented with systemic administration. However, it does not exclude the remote risk of idiosyncratic responses to any exposure6,15.
Chloramphenicol and testicular toxicity
Interestingly, in April 2021, the Royal College of Ophthalmologists (RCO) in the UK released a statement on chloramphenicol use, noting that drop preparations contain trace levels of boron, which has been associated with infertility in a rat model. The RCO’s quality and safety group noted: “Although more data on the concentration of borates in individual formulations of chloramphenicol are required, currently available data suggest that the recommended maximum daily dose of boron is unlikely to be exceeded with conventional eyedrop regimes, even for children under the age of two. At the present time, the college believes that the benefits of chloramphenicol eyedrops in paediatric ophthalmic practice for appropriate indications and with courses of appropriate duration outweigh the possible risks posed by boron ingestion.” However, some manufacturers have changed their labelling to state, “This medicinal product must not be given to a child less than two years old as it contains boron and may impair fertility in the future.”
Conclusion
The unprecedented level of concern about increasing antibiotic resistance reflects the growing frustration with the intractability of this multifaceted problem. It appears, however, to be less of a problem in ophthalmology in New Zealand at present, as intrinsically acquired bacterial resistance is generally not transmitted between ophthalmic (unlike respiratory) patients, and there are available antibiotics to treat resistance. In this context, the limitations of, and alternatives to, combination antibiotic-corticosteroid preparations should be carefully considered. As elucidated, indiscriminate use of these preparations for prophylaxis or the treatment of minor conjunctival infections contributes to the development of individual antibiotic resistance and increases the propensity to latent and secondary infections, as well as exposure to the myriad adverse effects of steroids. In New Zealand, the rate of antibiotic resistance is justifiably lower given the judicious use of systemic antibiotics and general adherence to guidelines.
With local studies demonstrating excellent sensitivity in common ocular microbes, coupled with its low cost and minimal irritative effect on the cornea, chloramphenicol remains the antibiotic of choice for postoperative prophylaxis.
References
- Fung AT, Tran T, Lim LL, Samarawickrama C, Arnold J, Gillies M, Catt C, Mitchell L, Symons A, Buttery R, Cottee L. Local delivery of corticosteroids in clinical ophthalmology: a review. Clinical & experimental ophthalmology. 2020 Apr;48(3):366-401.
- McGhee CN. Pharmacokinetics of ophthalmic corticosteroids. The British journal of ophthalmology. 1992 Nov;76(11):681.
- Roters S, Aspacher F, Diestelhorst M. The influence of dexamethasone 0.1% eye drops on plasma cortisol and ACTH concentrations after cataract surgery. Ophthalmologica. 1996;210(4):211-4.
- Howes J, Novack GD. Failure to detect systemic levels, and effects of loteprednol etabonate and its metabolite, PJ-91, following chronic ocular administration. Journal of ocular pharmacology and therapeutics. 1998 Apr;14(2):153-8.
- Wong T, Ormonde S, Gamble G, McGhee CN. Severe infective keratitis leading to hospital admission in New Zealand. British Journal of Ophthalmology. 2003 Sep 1;87(9):1103-8.
- McGhee CN, Anastas CN. Widespread ocular use of topical chloramphenicol: is there justifiable concern regarding idiosyncratic aplastic anaemia?. British journal of ophthalmology. 1996 Feb 1;80(2):182-4.
- Lockington D, Sharma R, Mantry S, Ramaesh K. Maxitrol-induced corneal melts after routine cataract surgery in rheumatology patients. Clinical & experimental ophthalmology. 2014 Sep 29;43(2):188-9.
- Park SH, Lim JA, Choi JS, Kim KA, Joo CK. The resistance patterns of normal ocular bacterial flora to 4 fluoroquinolone antibiotics. Cornea. 2009 Jan 1;28(1):68-72.
- Pandita A, Murphy C. Microbial keratitis in Waikato, New Zealand. Clinical & experimental ophthalmology. 2011 Jul;39(5):393-7.
- Rajpal K, Hall R, Long H, Wells A. Five-year experience of corneal scrapes at Wellington Eye Department, New Zealand. The New Zealand Medical Journal (Online). 2007 Aug 24;120(1260).
- Hall RC, McKellar MJ. Bacterial keratitis in Christchurch, New Zealand, 1997–2001. Clinical & experimental ophthalmology. 2004 Oct;32(5):478-81.
- Wallerstein RO, Condit PK, Kasper CK, Brown JW, Morrison FR. Statewide study of chloramphenicol therapy and fatal aplastic anemia. JAMA. 1969 Jun 16;208(11):2045-50.
- Fraunfelder FT, Bagby GC. Fatal aplastic anemia. JAMA. 1982 May 14;247(18):2499-.
- Doona M, Walsh JB. Use of chloramphenicol as topical eye medication: time to cry halt? BMJ 1995;310(6989):1217-18.
- Walker S, Diaper CJ, Bowman R, Sweeney G, Seal DV, Kirkness CM. Lack of evidence for systemic toxicity following topical chloramphenicol use. Eye. 1998 Sep;12(5):875-9.

Dr Aaron Ong is a clinical research fellow working with Professor Charles McGhee at the Department of Ophthalmology, University of Auckland.