Bandage Contact Lenses
As contact lens fitters, too often we find ourselves fixated over obtaining the very best visual results for our patients. These days we can specify a dizzying array of toric powers and axes into our soft daily lenses. We can incorporate spherical aberration correction and multifocal optics into our scleral lenses. Heck we can even customise an orthokeratology lens to match a child’s pupil size. It is all very empowering. Still, there is an important application for contact lenses where the power and vision through the lens is largely irrelevant: bandage contact lenses.
Bandage contact lenses (BCL) refers to the application of contact lenses, typically soft silicone hydrogel extended-wear lenses, for therapeutic reasons such as facilitating corneal healing or protecting a fragile corneal surface. The key concept of a bandage contact lens is the relentless shearing forces of our blinking lids is nullified during wear, often offering immediate relief to patients (and practitioner!) as soon as they are inserted.
The concept of a protective eye bandage originated several millennia ago when a smart chap called Celsus reportedly applied a honey-soaked linen to the site of a pterygium removal to prevent symblepharon development. Last century the technique of pressure-patching had traditionally been used when an eye needed protection to heal. Interestingly, a study several decades ago showed patients with traumatic corneal abrasions healed significantly faster, had less pain and had fewer reports of blurred vision when they were not wearing a pressure patch. Corneal abrasions due to removal of foreign bodies showed similar results¹.
Contact lenses were first used as an alternative to pressure patching following the development of hydroxyethyl methacrylate (HEMA) soft contact lenses in the 1970s. Bandage contact lenses were superior to patching for a number of reasons: vision could be maintained during wear, topical medications could continue to be instilled, and the cosmesis was far better. Let’s be honest, not too many people enjoy stepping out into the world with half a roll of gauze taped to their face! Today’s modern bandage contact lenses provide the same benefits as their predecessors - but with enhanced convenience, improved healing and better corneal health due to the high Dk materials we now use - an important consideration if extended wear is required.
The choice of lens design depends on a few factors but, typically, a lens with a low modulus is preferred as these will drape onto the underlying tissue better and theoretically provide less mechanical interaction. My preferred lenses are those with a modulus below 0.8 MPa such as Biofinity (Coopervision) for a monthly lens and the fortnightly CAir (Coopervision) or Acuvue Oasys (J&J) if a shorter duration of wear is expected. For comparison, the Air Optix (Alcon) and Purevision (Bausch + Lomb) lenses are made of stiffer materials with a modulus above 1.0 MPa. I have spoken with several clinics using these high modulus lenses as BCLs and they report few issues. If a custom bandage lens is required the SiHg Definitive 74 material has a reasonable Dk of 60 Fatt units and a nice low modulus of 0.4 MPa.
There are a number of reasons to use a BCL:
- Protection: BCLs can offer convenient protection of the ocular surface in the case of entropion, trichiasis, tarsal scars, recurrent corneal erosion and in the presence of exposed surgical sutures or knots.
- Pain relief: Reducing patient discomfort is a useful application for a therapeutic contact lens. Conditions like bullous keratopathy, epithelial erosion or abrasion and filamentary keratitis can be debilitating without a contact lens in place. In the case of bullous keratopathy failure of the endothelium leads to swelling of the cornea and formation of epithelial blisters that can painfully rupture over time. A BCL reinforces the damaged tissue and protects the nerve endings from the abrasive actions of the eyelids. They can also make the wait for an endothelial graft more tolerable.
- Healing: The use of a BCL to improve the healing response of the cornea is particularly valuable in a number of conditions including chronic epithelial defects, neurotrophic keratitis and chemical burns. BCLs also play an important role following corneal surgery, particularly photorefractive or phototherapeutic keratectomy (PRK/PTK), and following corneal cross-linking. In these procedures, the epithelial is chemically removed and can take up to a week to heal. A BCL provides a protective scaffolding for the limbal epithelial cells to redistribute centrally.
Let us also not forget the role the fluid reservoir of a rigid scleral lens can play in protecting and healing the fragile ocular surface in chronic dry eye conditions. A study led by Romero-Rangel² described the therapeutic benefits of scleral contact lenses to patients with conditions including Stevens-Johnson syndrome, ocular cicatricial pemphigoid and Sjögren's syndrome. Improvement in quality of life as a result of a reduction in photophobia and discomfort was reported by 92% of the patients studied. At contact lens conferences, I have come across reports of extended wear scleral lenses being used effectively to rehabilitate non-healing corneal ulcers. Sleeping in these lenses, however, created significant hypoxic oedema, requiring careful consideration of the risk-benefit in extreme cases.
- Sealing: BCL also play a role in sealing leaky wounds. A leaking bleb following trabeculectomy surgery is a serious complication and has been reported to be more likely with the popularity of anti-fibrotic agents like 5-FU and mitomycin-C, occurring in 5-30% of surgeries³,⁴,⁵,⁶. Blebs can be sealed with a BCL although customised larger diameter lenses are typically required to cover the area. At Greenlane Clinical Centre, optometrist Reuben Gordon tells me the team use the amusingly nick-named ‘Floppy Johnson’ (presumably named after its pendulous designer) custom soft lens for this purpose. The Floppy Johnson has a flat base curve of 8.9mm and large diameter of 16mm and is well loved by the glaucoma surgeons as a bleb sealer. Literature results are favourable demonstrating a 92% success rate using 17.50mm soft bandage contact lenses for this purpose⁷.
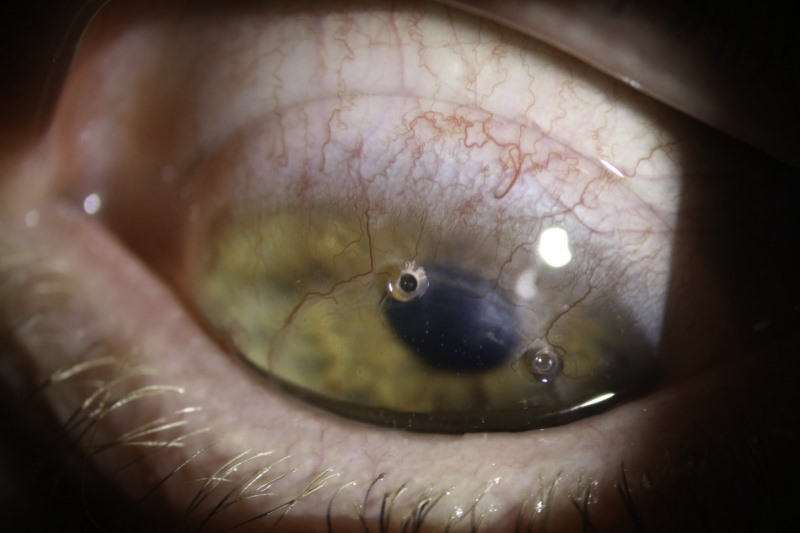
Several good examples of the benefits of bandage contact lenses have arisen in my clinic in recent months. The first was the case of an electrician in his thirties who flicked a coil of wire into his eye the day before presenting to me (Fig 1). Unsurprisingly, the eye was sore, watery and photophobic, but it felt like it was improving as the day went on. Examination revealed an anterior stromal laceration to about 50% thickness with a narrow, almost dendritic, epithelial defect that appeared to be healing already. Vision was excellent, there was no infiltrate and the anterior chamber was quiescent. The patient was prescribed regular prophylactic chloramphenicol ointment with a review planned later in the week.

Fig 1. Beware malevolent coils of wire
Unfortunately, the patient returned the next day as, on waking, his eye suddenly felt significantly worse. On re-inspection, the epithelial defect had widened, presumably due to the actions of the lids. A bandage SiHg soft contact lens (CAir +0.25D) was inserted which gave immediate relief. He was asked to use this lens for extended wear with prophylactic chloramphenicol drops four times a day. One week later the eye was feeling much better. On removal of the bandage lens (taking care to lubricate the eye and the lens with a drop of artificial tears before removal to avoid re-aggravating the fragile surface) the epithelial defect had healed beautifully (Fig 2). The stromal laceration was still evident as we would expect this tissue layer to take longer to heal fully.
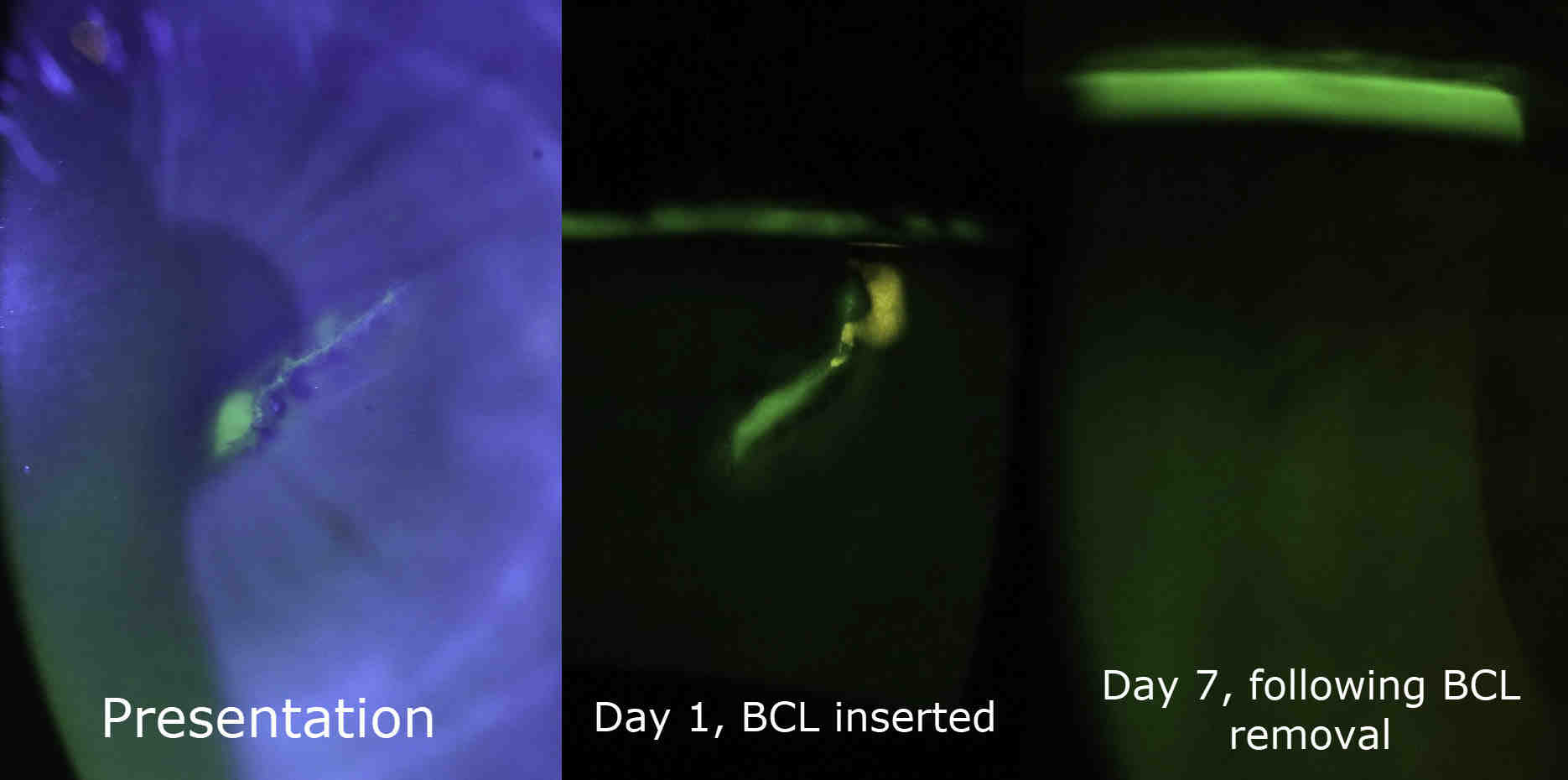
Fig 2. The epithelial defect resolving with extended wear use of a BCL
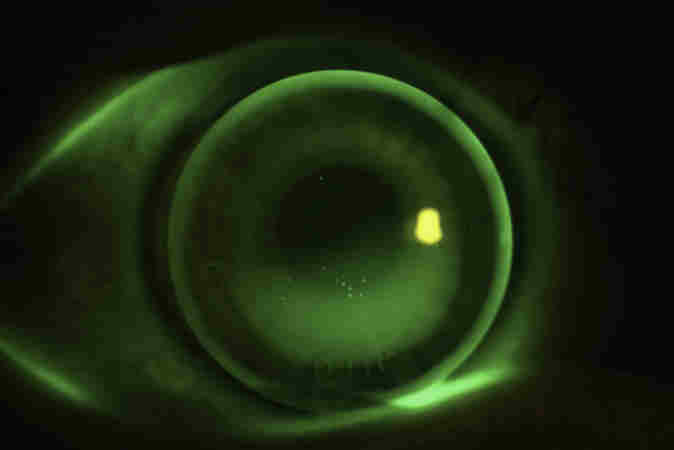
My second example is a young chap in his twenties with severe meibomian gland dysfunction and secondary evaporative dry eye (Fig 3). He was referred to my clinic by ophthalmology for dry eye management. After treatment with oral azithromycin, intense-pulsed light treatment, omega-3 supplements and regular hot compresses and digital meibomian gland expression we were able to wean him off the FML drops he was dependent on at presentation. His eyes felt less dry and he did not need to use his non-preserved lubricants as often. However, his right eye still had a significant area of confluent corneal epitheliopathy inferiorly that had not improved over the course of six weeks (Fig 4). His tarsal conjunctiva had a very inflamed appearance, which was most likely contributing to the chronicity of the epitheliopathy, in much the same way a shield ulcer forms in vernal keratoconjunctivitis.

Fig 3. Severe meibomian gland dysfunction with lid wiper epitheliopathy and tarsal inflammatory conjunctivitis
I applied an extended wear bandage contact lens (CAir) to the eye and reviewed him one week later. The patient reported his eye had never felt better! The epitheliopathy had mostly resolved (Fig 5) and crucially the patient found the lens easy to wear all day long with only occasional lubrication. Interestingly this patient had been told that due to his MGD he could not wear contact lenses for his low myopia. We have now fitted this patient successfully into daily contact lenses (Proclear 1 day), that he removes for sleep. I received an email from him the other day: “Both of my eyes have been feeling excellent since I last saw you. I have been wearing the daily contacts most days and have felt relief even without the contact lenses.”
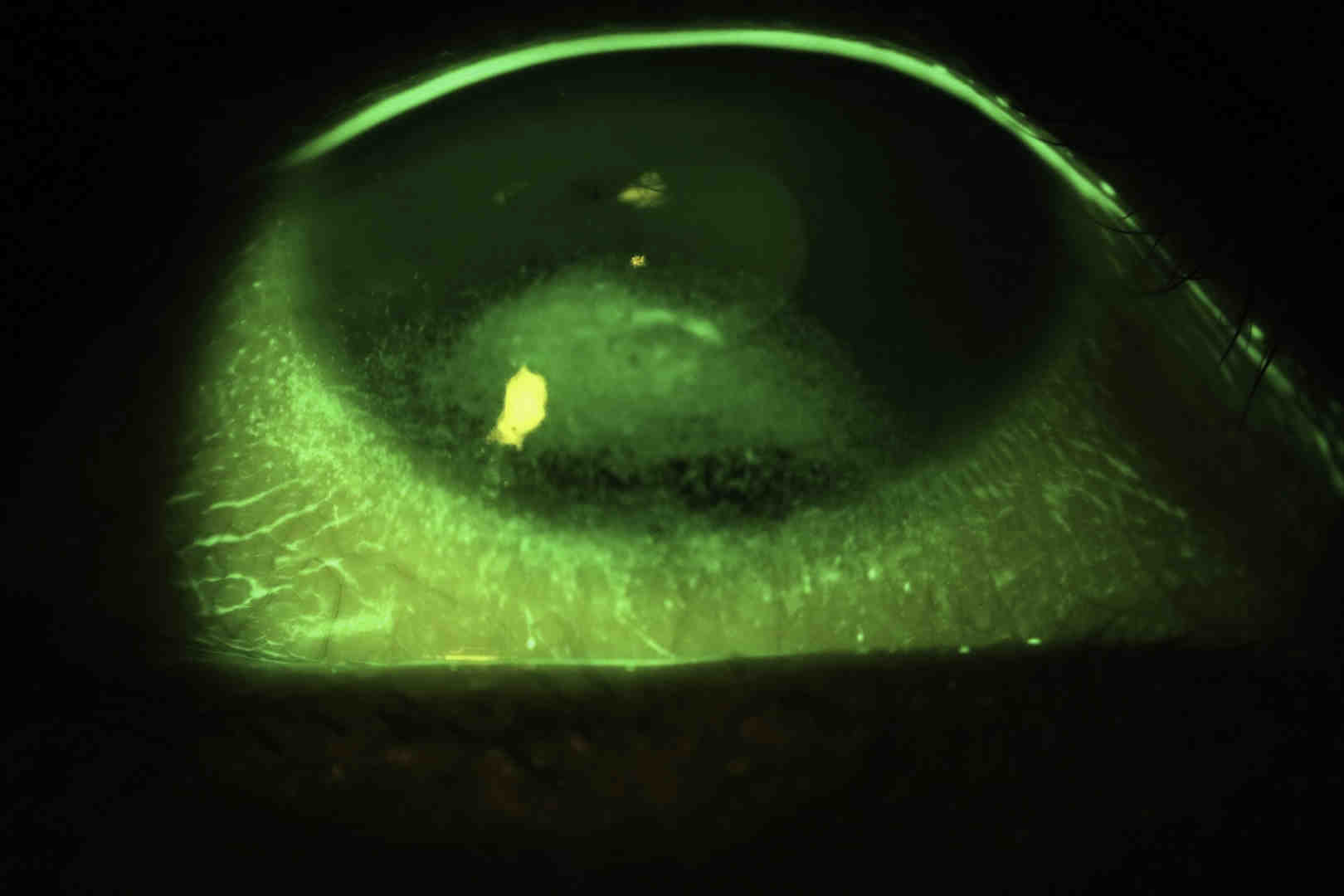
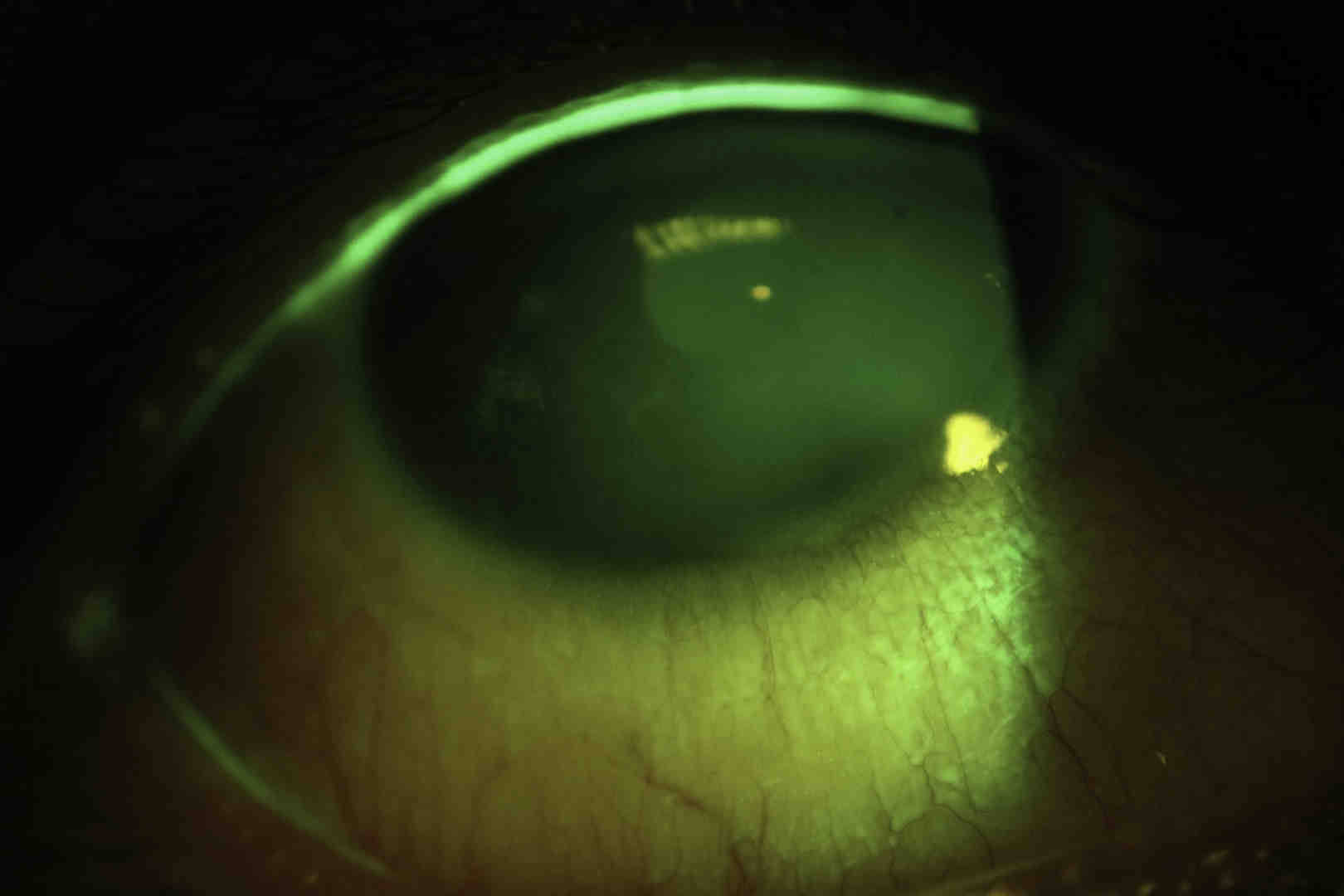
Fig 4-5. Resolution of a significant patch of confluent epitheliopathy in an MGD patient with a BCL
So, next time you are confronted with a troublesome ocular surface, consider reaching for a trusty bandage contact lens. You will be impressed how successful this management can be for your patients. Always be mindful of the risk of infection, however, especially in a case with a significant epithelial defect.
That’s all from me for another year. Thank you to those with positive comments about the columns, it is always nice to hear that people have learnt something or changed how they practice to ultimately help their patients. I look forward to bringing you more thrilling specialty contact lens escapades in 2018. Happy holidays and happy contact lens fitting!
References
- Kaiser PK A comparison of pressure patching versus no patching for corneal abrasions due to trauma or foreign body removal. Corneal Abrasion Patching Study Group. Ophthalmology. 1995 Dec;102(12):1936-42.
- Romero-Rangel T, Stavrou P, Cotter J, et al. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol 2000;130(1):25-32.
- Mandal, AK. Management of the late leaking filtration blebs. A report of seven cases and a selective review of the literature. Indian J Ophthalmol. 2001;49:247
- Schuman, JS. Zaltas, MM. Management of the leaking bleb. In:Ritch R, Shields, MB. Krupin, T. editors. The Glaucomas. 2nd edition. St. Louis; C.V. Mosby Company 1996, pp 1737-44.
- Ticho, U. Ophir, A. Late complications after glaucoma filtering surgery with adjunctive 5-fluorouracil. Am J Ophthalmol 1993;115:506-10.
- Katz, GJ., Higginbotham, EJ. Lichter, PR, et al. Mitomycin C versus 5-fluorouracil in high risk glaucoma filtering surgery: Extended follow-up. Ophthalmology 1995;102:1263-69.
- Shoham, A. Tessler, Z. Finkleman, Y. Lifshitz, T. Large soft contact lenses in the management of leaking blebs. CLAO J 2000 Jan;26(1):37-39.
About the author
Alex Petty (BOptom hons, FIAO) is a New Zealand optometrist based at Bay Eye Care in Tauranga, with a particular interest, knowledge and passion for speciality contact lenses, ortho-k and myopia control.