Bridging the gap with macular patients
A recent UK study comparing patient and eyecare professional (ECP) views about information provided on age-related macular degeneration (AMD) and diabetic macular oedema found a distinct difference between what ECPs think they tell patients and what patients remember.
Published in Eye and conducted by the UK Macular Society and research firm Yellow Insights, the study found 68% of ECPs said they always give patients information about macular disease at the point of diagnosis. However, only 21% said they consistently provide information to patients considered at-risk of developing the condition. In contrast, only 56% of patients said they received a clear diagnosis (including the name of the condition) at the time they were diagnosed, 45% said they received an explanation of what may happen to their vision in the future and just 17% of those surveyed said they recalled receiving information about support services. As many as 63% of patients said they did not know their symptoms were due to macular disease (during the diagnostic process) and 25% did not think those symptoms were important.
Bridging the gap
Sarah Berman, general manager of Macular Degeneration New Zealand (MDNZ) said when patients reach out to the charity, staff often detect a knowledge gap about their condition. It’s difficult to know the reasons behind it though as no formal analysis has been undertaken here, she said. “Most patients who contact MDNZ know whether they have wet or dry AMD but may not know the detail of their disease.”
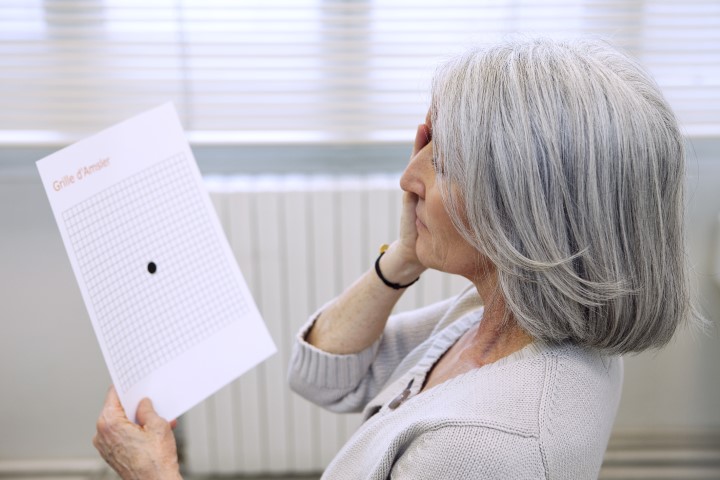
For example, a patient who recently approached MDNZ had been told by his optometrist he had dry AMD but he did not know it could turn into wet or that he needed to use an Amsler grid to help monitor any changes, said Berman. “As it happened, his AMD did turn into wet and – thanks to his call to our helpline and the Amsler grid we sent him – he was informed and contacted his ECP immediately. It saved his sight.”
MDNZ has long been concerned that the message of early detection, intervention and support isn’t as widely shared as possible, said MDNZ trustee Dr Ainsley Morris. “To this end, surveys of what percentage of the population know what macular degeneration (MD) is were undertaken in 2018, 2020 and again in 2024. Our target is 80% awareness of MD for those over 50 years of age and it currently sits at 55%. The sooner a patient presents, the more effective and supportive their treatment can be.”
Patient education is very important, agreed MDNZ trustee John Adam. “Often in practice people do not take everything in that they are told, so partnering with a team like MDNZ can aid in patient education. MDNZ has the resources and information patients like to see and can be an adjunct to your practice.”
The new online registration form can help ECPs work with MDNZ to provide information packs for patients, providing another level of support, he said. “If you become a ‘professional friend’ of MDNZ you can have access to these packs within your practice environment. I believe it behoves us to supply all the information to patients at all times and MDNZ can help in our complete care for a patient.”
Tailoring the message
To ensure the message is understood by patients, practitioners need to deliver it in a manner that’s appropriate to that specific patient, said Dr Morris. “This might mean a different language (oral or sign) and ensuring that you allocate enough time for the consultation, including an interpreter if you know one will be needed.” It also might mean tailoring your own diction to the specific situation and, most importantly, checking in with the patient to ensure they have correctly understood, she said.
Giving your patient ownership of the result, by showing them their photos and OCT results at the time of consultation, is incredibly powerful in ensuring they understand the diagnosis and the path forward, said Dr Morris. “All of us should also be open to having anyone the patient wants present at the consultation. Sadly, time constraints exist in all practices so if there isn’t enough time there’s nothing wrong with scheduling another appointment to devote more time to the patient – this can also be an excellent method of checking what your patient has understood.” Dr Morris said it’s also standard practice, and something she always does, to copy a patient into any correspondence to facilitate a better understanding and provide a better shared treatment model.
To address the knowledge gap and save people’s sight, it is vital patients with MD are referred to MDNZ at their earliest diagnosis, said Berman. “We can fill in the gaps by explaining in the patient’s own time about the disease, how the health system works and what their options are. As well as the 0800 Macula helpline and emails, we also deliver awareness and education seminars around New Zealand so that patients can get detailed information and ask questions about the disease. We know that people absorb information differently, so we try and cater to everyone’s needs.”
To refer patients with macular degeneration visit here