DED treatment without the fancy equipment
New and exciting developments in dry eye diagnosis and management are constantly emerging, while skilled clinicians are making dry eye disease (DED) their specialty. All of this can start to make an optometrist feel like they no longer have the equipment, skill or time to treat DED, but this is not the case. Since community optometry is the best place to treat the bulk of these cases, before they get severe, there’s a plethora of DED patients who still need your advice, and a confident optom can do that without fancy equipment.
Streamlining your basic dry eye assessment
To make dry eye assessment part of your routine eye test, it has to be fast and use equipment that’s already in your exam room. Practice the assessment on lots of normal eyes and asymptomatic patients. Taking a really thorough history is key and could be the subject of an entire article on its own!
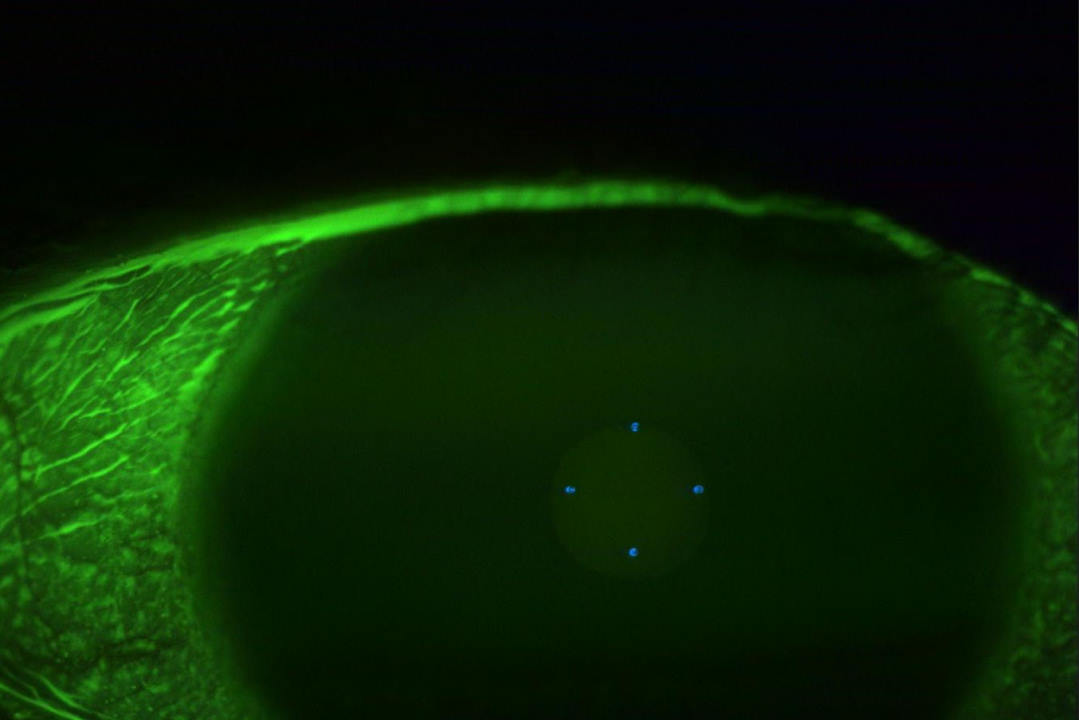
Sodium fluorescein
Assess for superficial punctate keratitis, tear break-up time (TBUT) and tear volume, by instilling a tiny amount of fluorescein – and use a yellow barrier filter if you have one. Take advantage of the visibility afforded by the fluorescein to pay attention to how thick the tear layer is for normal eyes – does it vary with blinks? Don’t waste too much time on counting the TBUT. Pick a value, say 10 seconds, and stop counting after that. Anything under five seconds is poor, 6-10 seconds is borderline and over 10 seconds is a normal, robust tear film1.
Slit-lamp observation
Look for lid margin staining, conjunctival staining and for signs of blepharitis, meibomian gland dysfunction and allergy. A dry eye can also have subtle allergic changes, so treating both is often the key to success.
Simplifying treatment options
Pick a favourite type of preservative-free artificial tears; get familiar with it and consider it the starting point for your DED management. You can always change it or add extra products to your treatment plan as you gain more experience. It might be the product your practice already uses, or one you’ve read about. The more familiar you get with your new treatment regime, the more comfortable you will be modifying it to each patient’s needs.
Begin by recommending a specific dosing, say four times a day, to try to nip symptoms in the bud. Avoid ‘as required’, particularly in the early stages, as it’s a bit vague and patients can interpret that to mean the artificial tears aren’t essential.
While offering verbal instructions makes a lot of sense, it’s helpful to follow up with written information that patients can review later. Sometimes I’ll send the patient an email summarising their treatment plan, especially if I’ve made changes to their regime. For first-time patients I have a handout explaining the different types of dry eye and all the treatment options (drops, ointments, oral supplements, warm compresses and also referable options like LipiFlow or intense pulsed light); I highlight the treatment options we’re starting with. This can give the patient hope if our first choices don’t achieve the desired results.
As you get better at spotting evaporative dry eye over aqueous deficiency you can refine your approach to recommending treatments such as oil-based eye drops. I also find that gels and ointments can be most effective with overnight use for patients who tend to wake with dry eyes, as well as Optimel manuka honey products for patients with lid margin staining, telangiectasia and those with raw, red eyelids. Over time, patient feedback will lead you to recommend different brands for different scenarios. One bottle might be too big for their pockets or too tricky to get in the eye. Convenience plays a big part in compliance.
I hope some of these tips will help get your dry eye assessment more streamlined and stress-free!
This article is a condensed version of Shannon Tubman’s March 2023 presentation at the Cornea and Contact Lens Society of New Zealand conference in Auckland. For more information on taking a simplified approach to dry eye management, click here.
Reference
1. Pauk S, Petriček I, Jukić T, et al. Noninvasive tear film break-up time assessment using handheld lipid layer examination instrument. Acta Clin Croat. 2019 Mar;58(1):63-71

Shannon Tubman is an optometrist, assessing patient suitability for laser vision correction and helping with post-surgery recovery at the Wellington Eye Centre.