Demodex mites – how well do you know them?
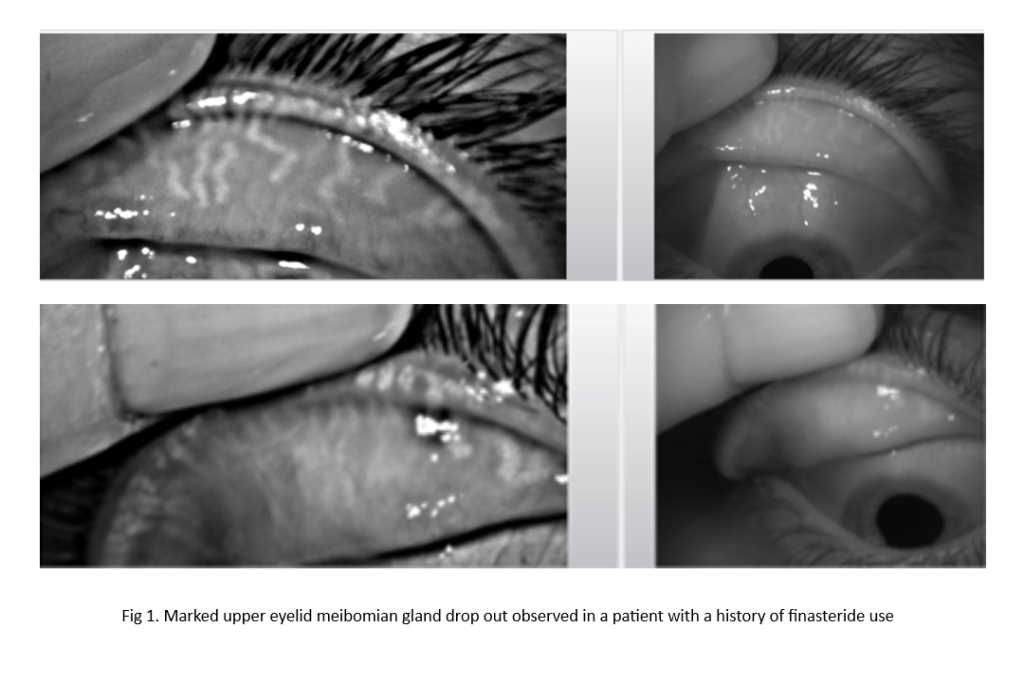
Demodex blepharitis remains an under-diagnosed condition, lacking universally accepted diagnostic and management protocols. Two species, Demodex folliculorum and Demodex brevis, have been reported to infest humans causing a recurrent chronic form of blepharitis¹,². The former is found in eyelash follicles while the latter resides in the meibomian glands³.
Demodex blepharitis has been associated with various ocular surface diseases such as dry eye disease (DED), meibomian gland dysfunction (MGD) and chalazion. These conditions can reduce patients’ quality of life and induce anxiety, depression and lack of self-esteem. The exact aetiopathological mechanism remains unknown since these mites are also found in healthy individuals and, therefore, the pathogenicity is highly debated in the literature⁴,⁵. Moreover, the multifactorial nature and overlap in signs and symptoms with other ocular surface diseases could mislead eyecare practitioners, delay diagnosis and result in inappropriate treatment.
Alongside our Glasgow Caledonian University colleagues Drs Ian Pearce and Suzanne Hagan, plus Professor Christine Purslow (Cardiff University), and in collaboration with Professor Jennifer Craig at the University of Auckland, we recently conducted a study comparing practitioners’ perspectives on Demodex blepharitis⁶. Ophthalmologists and optometrists from India, Australia and New Zealand were invited to complete an online survey. Practitioner demographics and views on eyelid health in general, as well as details of diagnostic and management practices (from those reporting that they treat Demodex blepharitis in clinical practice), were collected. A total of 261 eyecare professionals – 207 from India (84% optometrists, 16% ophthalmologists) and 54 from Australia and New Zealand (91% optometrists, 9% ophthalmologists) – completed the survey.
Differing approaches
Overall, the study highlighted differences in clinical evaluation and treatment practices between India and Australasia. In both regions, interprofessional differences in perceived optimal treatment duration and frequency were observed. Almost 70% of practitioners across the three countries considered Demodex blepharitis to be a cause of ocular discomfort, yet only 45% reported attempting to identify the presence of Demodex clinically in their patients, although a greater number of Australasian practitioners reported attempting to do this, compared with their Indian counterparts (85% vs 35%). Practitioners’ views differed in terms of the perceived prevalence of Demodex blepharitis (60% in Australasia vs 27% in India). There were also differences in the choice of slit lamp magnification used for a general view of the lids/lashes (10x in India vs 16x in Australasia) and choice of slit lamp magnification to detect the mites (16x in India vs 25x in Australasia). Preferred treatment options (tea tree oil in Australasia vs standard lid hygiene in India), duration (3-4 weeks to more than 12 weeks in Australasia vs 3-4 weeks in India), and frequency (once a day in Australasia vs twice a day in India) were also observed.
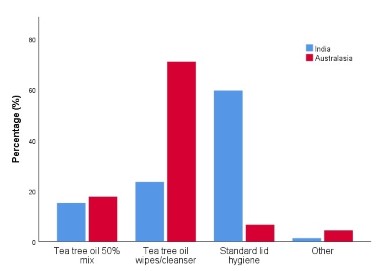
Comparison of Demodex blepharitis treatment practices in India and Australasia
There are differences in the way Demodex blepharitis is diagnosed and managed around the world. This may be a result of different training programmes and upskilling of practitioners, leading to different levels of knowledge on the subject. The results from this study highlight a need for standardised treatment protocols to be developed for managing patients with Demodex blepharitis. More research on this topic is required to find out the best evaluation and treatment techniques, so that internationally approved guidelines can be developed and disseminated for better and more consistent patient care around the world.
Clinical take-home messages:
- Demodex can be identified clinically under the slit-lamp using high magnification (25x-40x)
- Cylindrical dandruff at the base of the eyelash correlates well with over-population of Demodex
- While various new treatment options are in development, tea tree oil (TTO) in a dose-dependent manner remains the most favoured clinical option to manage Demodex blepharitis. However, high concentrations of TTO may not be well tolerated by patients
References
1. Cheng A, Hwang J, Dermer H, Galor A. Prevalence of ocular demodicosis in an older population and its association with symptoms and signs of dry eye. Cornea 2021;40(8): 995-1001.
2. Zeytun E, Karakurt Y. Prevalence and load of demodex folliculorum and demodex brevis (acari: Demodicidae) in patients with chronic blepharitis in the province of Erzincan, Turkey. J Med Entomol 2019;56(1):2.
3. Bitton E, Aumond S. Demodex and eye disease: A review. Clin Exp Optom. 2021;104(3):285-294.
4. Biernat M, Rusiecka-Ziółkowska J, Piątkowska E, Helemejko I, Biernat P, Gościniak G. Occurrence of demodex species in patients with blepharitis and in healthy individuals: A 10-year observational study. Jpn J Ophthalmol 2018;62(6):628-33.
5. Zhang A, Muntz A, Wang M, Craig J, Downie L. Ocular demodex: A systematic review of the clinical literature. Ophthal Physiol Opt 2020;40(4):389-432.
6. Sharma N, Martin E, Pearce I, Hagan S, Craig J. Practitioners’ perspectives on demodex blepharitis: A comparison between eye care practitioners in India and Australasia. Invest Ophthalmol Vis Sci 2022;63(7):3945–A0225.

Nikhil Sharma is a full-time PhD candidate at Glasgow Caledonian University. His research focuses on investigating the role of Demodex mites in ocular surface inflammation and dry eye disease.

Dr Eilidh Martin is a lecturer in Vision Sciences at Glasgow Caledonian University. Her teaching and research focuses on contact lenses, dry eye disease and blepharitis.