Hard graft at the 2023 ANZ Cornea Society meeting
I was privileged to attend the 38th ANZ Cornea Society and Eye Bank Meeting in Perth, the first in-person meeting since 2020, together with New Zealand’s National Eye Bank team, including director Dr James McKelvie and Dr Bia Kim, a senior anterior segment fellow at Te Whatu Ora Auckland. As well as covering advances in corneal surgery, this year’s meeting was also an opportunity to update surgeons and eye bank members on the trend changes for corneal tissue use in surgery and tissue donation post-Covid. It was an illuminating glimpse into the intricacies of eye bank coordination in the fight against blindness.
Erik Hellier, director of global development for Eversight, a US network of non-profit eye banks, outlined the company’s difficulties in sourcing corneal tissue overseas. Hellier was involved in setting up a South Korean eye bank to create a more central hub to distribute tissue farther. He noted the criteria for tissue donation had become stricter with the introduction of further tissue testing, including for syphilis. Compounding the issue, the high cost of manufacture and company insolvencies in the wake of Covid led to limited supplies of tissue-storage media.
Expanding on Hellier’s concerns, Pierre Georges, coordination team leader at Lions NSW Eye Bank, discussed a recent study showing the lack of conversation about eye tissue donation by optometrists and ophthalmologists. Although most eyecare professionals said they were comfortable talking about the subject when raised, it didn’t always feel appropriate or they hadn’t enough consulting time, he said. Patient factors included family refusing donation, a lack of knowledge about donation and not wanting to donate eyes specifically. It was pointed out that some willing potential donors and their families were incorrectly told by a hospital doctor they were not candidates, based on their other organs’ unsuitability for donation.
Shifting graft trends, increasing demand
Dr Miriam Keane, executive director of the Australian Corneal Graft Registry (ACGR), discussed the changing trends of the last two decades. Unsurprisingly, there has been an increase in endothelial keratoplasties, with Descemet's stripping (automated) endothelial keratoplasty, Descemet's membrane endothelial keratoplasty and penetrating keratoplasty having roughly equal numbers performed in 2020. As the region recovers from Covid, ACGR is expecting the demand for grafts to increase in 2023, she said.
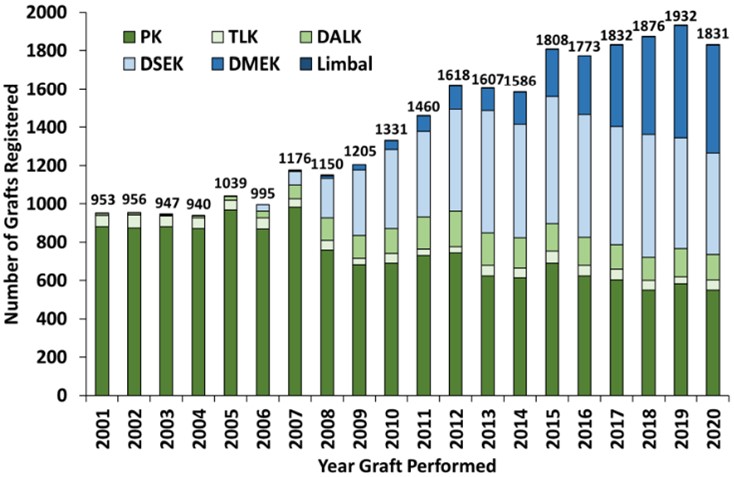
Fig 1. Number of annual grafts registered with ACGR, 2001-2020
Interesting new techniques with corneal graft involvement were also covered by Dr David Gunn, a corneal and refractive specialist in Brisbane. He described corneal allogenic intrastromal ring segments (CAIRS) for keratoconus, which replace intracorneal ring segments (ICRS) by using ring implants from corneal donor tissue instead of keraring implants. A case series showed promising results, he said, with only one patient requiring further laser eye surgery for refractive correction. The benefits of donor tissue over keraring implant include biocompatibility, stability with reduced migration and minimal risk of extrusion, plus greater customisation for patients.
Dunedin-trained Dr Hong Sheng Chiong, a senior anterior segment fellow at Sydney Eye Hospital Foundation and co-founder of oDocs, shared his experience of patch endothelial keratoplasty for corneal perforations. The technique involves introducing a smaller circular endothelial graft via the anterior chamber and covering the perforation internally, through a larger corneal paracentesis. Good results have been achieved so far, which his group is hoping to publish. Our very own Dr Kim then talked about the management of endothelial graft dehiscence, with one corneal consultant adding endothelial glue to the mix.

Dr Hong Sheng Chiong
This year’s Douglas J Coster lecture was given by the University of Sydney’s Professor Gerard Sutton, while Professor Graham Barrett, from the University of Western Australia and Lions Eye Institute, delivered the John Blandford lecture. Prof Sutton used the opportunity to update us on the BIENCO (BIo ENgineered COrnea) consortium’s solution, which is awaiting the results of a further grant application to progress to the next stage of development – our fingers are crossed! Prof Barrett discussed his Barrett Universal II and Barrett True K formulae in cataract surgery.
This was my first Cornea Society and Eye Bank Meeting and I found it incredibly informative. It was special to be among a pioneering group of surgeons aiming to eliminate blindness and it made me really appreciate the hard work that goes into managing an eye bank and the difficulties of tissue donation and supply. New Zealand relies heavily on overseas corneal donations, so if we take one thing away from this conference, it would be to promote eye tissue donation in our clinics – even a poster to prompt a conversation with a patient could make a world of difference.
Dr Lize Angelo is an HRC clinical research fellow in the University of Auckland’s ophthalmology department, headed by Professor Charles McGhee. She’s pursuing a PhD in diagnosing and treating keratoconus, including aspects of equity of access to services in Aotearoa.