Iatrogenic DED – do ECPs cause DED?
What? Me? Causing dry eyes? But how?
In addition to treating dry eye disease (DED), many medical professionals, including eyecare providers, may be causing dry eyes. The primary ways we are increasing the prevalence of DED and ways to reduce these effects are listed below.
Contact lenses
Contact lens (CL) use has been associated with dry eye symptoms in many studies, although distinguishing between CL discomfort and dry eye is difficult due to overlap in symptoms. There are many changes in the tear film secondary to CL wear, including: increased tear evaporation rate, increased osmolarity, decreased tear meniscus volume and lower tear turnover rate. Specific alterations have been identified, including changes in corneal Langerhans cells and conjunctival goblet cells, lid wiper epitheliopathy and meibomian gland dropout. In addition, CL-induced inflammation may play a role at a cellular level and may be generated through mechanical friction as well as a stagnant tear film with accumulation of debris, metabolic by-products and bacterial exotoxins.
Management - Ensure ideal fit of CLs, use daily disposable CLs, CLs with internal wetting agents or designed for dry eyes, supplement with topical wetting agents, reduce CL wearing time.
Systemic medications
A large number of systemic medications have been associated with DED. The classes of medications associated with DED based on large epidemiological studies include antihypertensives, diuretics, NSAIDS, analgesics, antiulcer agents, sulfonylureas (for diabetes), cardiac glycosides, anxiolytics/benzodiazepines, anti-infectives, antidepressants, antihistamines, corticosteroids, hormone replacement therapy for women, anti-androgen therapy (for prostatic hypertrophy) and multivitamins, plus many others suspected of playing a role.
Various means have been proposed for how they cause or exacerbate DED. Some, such as aspirin, are secreted directly into the tears and may cause mechanical irritation or increased tear evaporation. Others, such as anticholinergics, may have a direct effect on the lacrimal gland and mucus-producing cells, thus reducing the aqueous and mucous components of tears. Others, such as diuretics, lower blood pressure by reducing the fluid load in the body, thereby indirectly affecting the eyes. One medication, in particular, that may be used by younger patients, is retinoic acid, or isotretinoin, which is used to treat acne and is suspected of causing atrophy of the meibomian glands resulting in severe chronic DED years later.
Management – As eyecare providers, we typically wouldn’t change a patient’s systemic medication that we’ve not prescribed. However, we can educate the patient that their DED could be worsened by some of their systemic medications and they should work with their GP to replace or reduce any non-essential medications.
Topical medications
A large number of eye drops have been associated with DED. The most commonly prescribed of these are glaucoma drops, particularly those containing preservatives, of which every class has been implicated. Dry eye symptoms have been identified in over 50% of those on glaucoma drops. Various mechanisms have been described including allergic, toxic and inflammatory effects, as well as disruption of the tear film through detergent effects, and direct damage to the corneal or conjunctival epithelia or meibomian glands. Additionally, treated eyes with glaucoma have reduced sub-basal corneal nerve density, increased nerve tortuosity and possibly decreased corneal sensitivity.
Many preservatives are used in ophthalmic preparations to reduce microbial contamination after a bottle is opened, most commonly benzalkonium chloride (BAK). BAK has cytotoxic, neurotoxic and pro-inflammatory effects on the ocular surface, and detergent effects on the lipid layer of the tear film. Newer preservatives developed as alternatives to BAK may have less severe cytotoxic effects.
Management: Reduction in the number of preserved drops applied daily may reduce the adverse effects. When possible, eye care providers should switch to preservative-free eye drops or combinations drops. Individuals with glaucoma may benefit from selective laser trabeculoplasty or other procedures to reduce the overall drop burden.
Ocular surgery
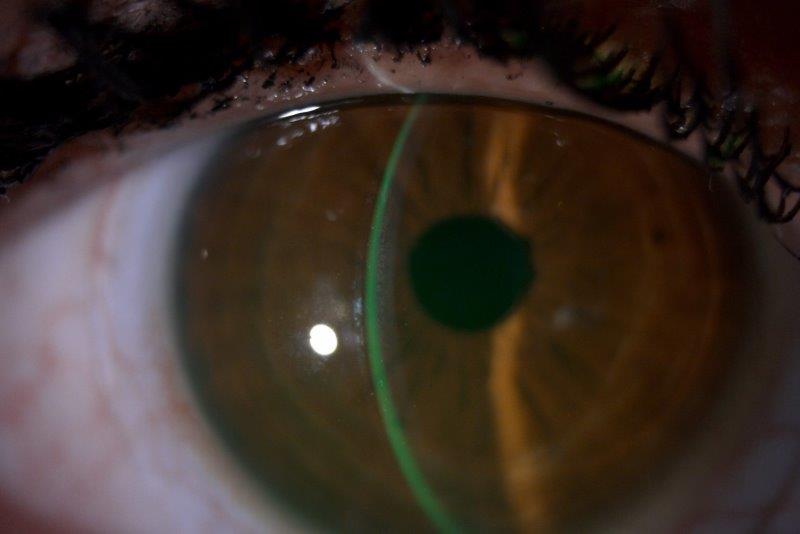
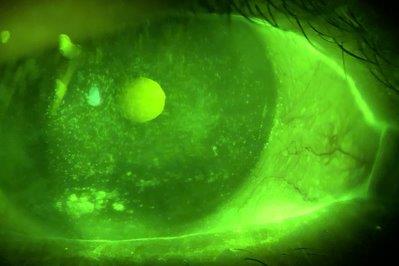
Nearly all ocular surgery has been associated with DED, including corneal refractive surgery, cataract surgery, keratoplasty, corneal cross-linking, lid surgery, vitreoretinal surgery, glaucoma surgery and conjunctival surgery. Following corneal surgery involving ablation or surgical transection of the nerves, there is a neurotrophic component of DED due to changes in corneal nerve density and corneal sensation. This is often transient, lasting several months, due to regeneration of the corneal nerves with time, although it can persist in a small number of patients. Other mechanisms involved with cataract surgery and other ocular surgeries include exposure to topical anaesthetics and antiseptics, exposure desiccation, generation of inflammatory factors, loss of conjunctival goblet cells and use of postoperative drops. Lid surgery, particularly blepharoplasty, can cause lagophthalmos and exposure (Fig 1).

Fig 1. Lagophthalmos following a blepharoplasty resulting in exposure keratopathy and microbial keratitis of a corneal graft
Management - Patients with pre-existing dry eye should be warned prior to surgery that this may worsen with surgery and steps should be taken to optimise the ocular surface beforehand.
Postoperatively, standard dry eye treatments are employed although anti-inflammatory treatments such as topical corticosteroids or cyclosporine may offer benefit in managing any residual inflammation.
Cosmetic treatments
Eyelid procedures such as eyeliner tattooing, eye cosmetics and botulinum toxin (‘Botox’) can all affect the ocular surface. Eyelid tattooing can induce loss of meibomian glands and shorten the tear breakup time. Eye cosmetics, including powders, mascara, eyeliner and creams may directly affect the tear film (sometimes particles are even seen in the tears on slit lamp examination) while retinoids applied to the lids may affect meibomian gland function. Botulinum toxin can affect the blink tone/strength and function and may cause lagophthalmos and exposure.
Management - Most commonly, products such as eyeliner that can contribute to meibomian gland dysfunction may be discontinued or their frequency of application reduced if the patient is willing. Paying attention to the ingredients used in cosmetics, avoiding the sharing of cosmetics and observing expiration dates is also recommended.
References
- Gomes, JAP, et al. Ocul Surf. 2017;15(3):511-518.
- McMonnies CW. Eye Vis. 2021;8(1):12.
- Cruzat A, et al. Ocul Surf. 2017;15(1):15-47.
- Wang MTM and Craig JP. Clin Optom. 2018;10(4):33-40.
Dr Jay Meyer is a subspecialist in cornea/external diseases and glaucoma. He is a consultant ophthalmologist at Eye Institute and the Auckland District Health Board and a senior lecturer at the University of Auckland.