Low-dose atropine for myopia? The jury’s still out!
With decades of conflicting studies on low-dose atropine’s efficacy in treating myopia and no Medsafe-approved drop available, are our young myopes missing out?
At the first International Conference on Myopia in New York in 1964, Dr Robert Bedrossian presented the results of his study ‘The effect of atropine on myopia’. The Vancouver ophthalmologist found that 75% of the eyes of 150 patients, aged seven to 13 years, showed no myopia progression following daily 1% atropine treatment over a one-year period, compared with only 3% of controls. But despite almost 60 years of studies and the debates that followed, consensus about atropine efficacy and dosage remains elusive.
“Right now, atropine is the only effective method to retard the progression of myopia and should be in optometry’s armament,” wrote Dr Jeffrey Cooper, clinical professor of optometry at SUNY State College of Optometry in a 2009 letter to Review of Optometry. Dr Cooper pointed out that every animal and human study since 1965, well performed or not, had come to the same conclusion: atropine is an effective medication in slowing down the progression of myopia. “The mean rate of progression of patients with myopia is 0.50D per year, while patients on atropine had a progression rate of approximately 0.05D; a 10-fold decrease. Stated another way, a 1.00D myope at age six without treatment would most likely become a 6.00D myope by 16 years of age, while a patient on atropine would most likely become a 1.50D myope,” he said. The letter was written in response to Legerton and Chou’s August 2009 paper ‘Myopia regulation: myth or megatrend’, in which they said: “Atropine therapy is not appropriate for most children.”
In 2016, the Singapore Eye Research Institute’s ‘Five-year clinical trial on atropine for the treatment of myopia 2 (ATOM2)’ study concluded, “Over five years, atropine 0.01% eyedrops were more effective in slowing myopia progression with less visual side effects compared with higher doses of atropine.” ATOM2 was the institute’s second large, randomised study to assess the safety and efficacy of topical atropine in controlling myopia progression in children in Singapore. Its findings suggested low-dose atropine was going to be the myopia game-changer, said Corrina McElduff and Professor Ian Flitcroft, Ireland-based myopia data analytics firm Ocumetra’s director of public affairs and medical director, respectively, in Optician Online. “0.01% atropine offered the prospect of good efficacy at slowing myopia progression with few side effects and no rebound,” they said.
Prof Flitcroft’s own ‘Myopia outcome study of atropine in children (MOSAIC)’ paper in 2019, however, found significant effects on refraction and axial length in subjects of white ethnicity, but not in non-white participants. In fact, he wrote, the results – combined with those of the US- and Europe-based CHAMP (Childhood Atropine for Myopia Progression) trial, and the US-based MTS1 trial from the Paediatric Eye Disease Investigator Group (PEDIG) – raised almost as many questions as they solved. “From a safety and tolerability perspective, the trials all agree that once-a-day eye drops are acceptable and have an excellent safety profile, with no serious adverse events. From an efficacy point of view, the results are more mixed,” he summarised.
Safety is one aspect of low-dose atropine treatment that doesn’t appear to be in dispute. Dr Cooper’s 2009 letter pointed out that it has been prescribed in patients for years to control uveitis without any evidence of long-term side effects. And although Legerton and Chou argued the loss of accommodation and dilation associated with atropine treatment might affect academic and sports success, make the patient more sensitive to sunlight, or create mydriasis that would be socially unacceptable, they offered no support for these claims, said Dr Cooper. “In my experience, these problems are minimal with the use of progressives to eliminate the effects of paresis of accommodation and Transitions (photochromic lenses) to reduce the sensitivity to light. Of more than 40 (of my) patients who used atropine, I have had only one patient stop the treatment due to light sensitivity,” he said.
The major obstacle to atropine’s universal acceptance is the lack of a major pharmaceutical company doing due diligence to get FDA acceptance of the drop, said Dr Cooper. “Since atropine has generic status, no pharmaceutical company has a (financial) incentive to perform the clinical trials necessary to obtain market approval and then market it… Thus, the lack of standard of care is more likely financial in nature than clinical.”
Atropine in Aotearoa
Most New Zealand practices, both independents and corporates, are offering atropine treatment or referring patients to someone who provides it these days, said Alex Petty, director of Bay of Plenty’s Bay Eye Care. “We offer low-dose atropine – generally starting at 0.025%, as it’s well tolerated and supported by studies – as part of our treatment options.” But often patients prefer other methods of optical control, including ortho-k, multifocal soft contact lenses or the more recently released myopia-control spectacle lens options, such as Miyosmart (Hoya) or Stellest (Essilor lenses), he said. “Some patients have a combination of ortho-k and atropine if they have aggressive myopia.”
Petty said his practice starts many patients with a single atropine treatment, then adds it to their regimen if progression is still significant. “There is sometimes a discrepancy with axial eye growth and refraction control in the studies too, so ideally you need to be able to measure axial length in practice to monitor effectiveness.”
Without the means to measure axial length at his practice, Christchurch optometrist Andrew Kim said he refers suitable patients to a local ophthalmologist who manages myopia and prescribes atropine. “Overall, there is more evidence for low-dose atropine than against and, given its excellent safety profile, I think there is no real harm in prescribing it if there is a possibility of slowing down a child’s myopia. It's like dry AMD – we recommend the AREDS (Age-Related Eye Disease Studies) formulation for moderate to severe AMD as it may help but it’s not guaranteed.”
At the University of Auckland’s School of Optometry and Vision Sciences (SOVS), myopia progression management is an important topic, said SOVS head Dr Andrew Collins, with students able to offer several different options in clinic, including contact and spectacle lenses and low-dose atropine treatment. Currently, they offer 0.05%, 0.025% or 0.01% atropine solutions, based on their clinical judgement of the patient’s age and rate of progression, he said. “In general, they routinely prescribe the higher low-dose formulations of 0.05% and 0.025% atropine then reduce the dose while monitoring progression (particularly for axial length change) with the aim of minimising the risk of a rebound effect on cessation of treatment.”

Dr Andrew Collins
Is there any point in 0.01%?
Dr John Phillips, principal investigator at Auckland University’s Myopia Laboratory, said the jury is still out on the clinical efficacy of 0.01% atropine for slowing myopia progression, with the literature also split on whether it is more or less effective in Asian compared to European children.
The confusion primarily results from one of the first large randomised clinical trials in the US (Repka MX, Weise KK, Chandler DL et al, JAMA Ophthalmol. July 2023), which suggested 0.01% atropine does not slow the progression of myopia in low to moderate myopes when compared with placebo. Writing in Optometry Times, New England College of Optometry fourth-year student Kathleen Thai said the findings contradict many studies previously supporting the use of atropine 0.01% for myopia management, but most of these were conducted in East Asia where myopia prevalence is very high. “Due to the variability in results, it is hard to really decide whether to stop the use of atropine 0.01% completely… conducting studies that focused on atropine concentrations in a single race population will help clinicians to decide which specific concentrations to use with different cases,” she said.
Petty said he tends to quote the 2019 ‘Low-concentration atropine for myopia progression (LAMP)’ study most, which showed 0.025-0.05% are the most helpful concentrations. He notes, however, that the study was conducted in Chinese children.
The University of Houston’s Professor Mark Bullimore, who consults for several ophthalmic, surgical and pharmaceutical companies on myopia, told Dr Kate Gifford on The Myopia Exchange podcast in 2019 that some practitioners may have overly embraced the 0.01% atropine story after the ATOM studies. The first of these found that 1% atropine was effective in controlling myopic progression over two years but resulted in visual side effects which compromised treatment compliance, whereas the 0.01% ‘control’ concentration resulted in similar myopic control. Reminding listeners that in myopes, axial length and refractive error are closely related, Prof Bullimore said the studies actually showed there was no slowing of axial elongation with 0.01% atropine. “So the ATOM2 kids, who were on 0.01% atropine bilaterally, elongated by 0.4mm over two years – pretty much the same as the control eyes in ATOM1. So no effect on axial length, despite pretty robust effects on refractive error.”

Prof Mark Bullimore
In the invited commentary on the US Repka et al study in JAMA Ophthalmology, optometrist researchers Dr Jeffery Walline, from The Ohio State University College of Optometry, and Associate Professor Dave Berntsen, from the University of Houston College of Optometry, summed up the issue, reporting that of the six most recent randomised studies comparing atropine 0.01% with placebo for myopia control, four reported a significant slowing of myopia progression, but only three reported significant slowing of axial eye growth.
Compounding the issue
In Australia, Aspen Pharmacare’s Eikance 0.01% atropine drop has been approved by the Therapeutic Goods Administration since 2022. It’s available on prescription for children aged four to 14 when myopia progresses by one or more diopters per year. In New Zealand, however, Medsafe approval of a low-dose atropine drop is on hold pending an available commercial product. Until that happens, prescriptions for 0.01-0.05% atropine must be compounded from stock 1% atropine. However, there’s just one compounding pharmacy manufacturing it for the whole country, said Dr Rasha Altaie, paediatric and cornea ophthalmologist and University of Auckland senior lecturer. “The application for low-dose atropine is still with Pharmac. Until we get Medsafe approval, we cannot proceed further with the application.” This presents a chicken-and-egg problem, she said. “Until we get this sorted we cannot look into what is available in the market, regarding the delivery system and the dose.”
Christchurch paediatric ophthalmologist Dr Antony Bedggood agreed. “We need a Pharmac-funded, locally sourced product that is at least 0.02% so that it will be effective across the full range of young patients who are accurately diagnosed with progressive myopia.” Low-dose atropine manufactured in a single-dose unit and preservative-free is definitely the way to go, said Dr Atlaie. “Hopefully, we are not far away from this.”
Most optometrists in and around Auckland source their low-dose atropine formulation from Optimus Pharmacy, at a cost of about $150 for a three-month supply, said Petty, whereas some hospital pharmacies, including those in Palmerston North and Christchurch, appear to be able to formulate drops “for next to nothing.” The variability in cost could simply be due to how practices or pharmacies decide to bill for atropine, said Kim. “Pharmacies that are compounding these drops may decide to charge for their time or perhaps they are simply charging for fully subsidised 1% atropine, which leads to little or no bill.”
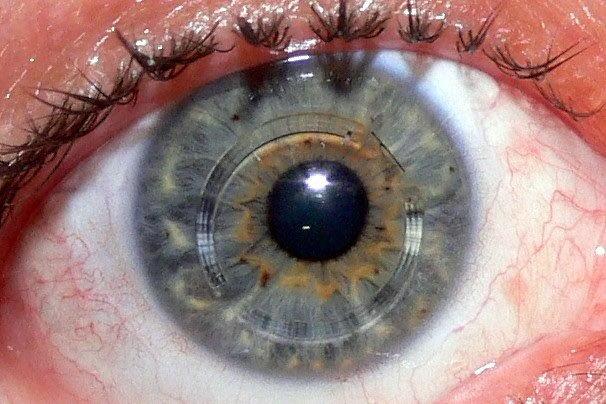
Costs aside, how low-dose atropine is formulated is a significant issue since it’s an unstable molecule, said Prof Bullimore on The Myopia Exchange. “There are papers from 50 to 60 years ago talking about the stability of atropine, which is pH dependent. So when you buy a bottle of 1% atropine, you’ll see it’s buffered between pH3 and pH6 – quite acidic. But when it’s compounded, it’s quite apparent from some informal enquiries that most compounding pharmacies are just diluting it and ignoring the pH. And that’s a problem!”
The variability in how much atropine actually survives compounding and subsequent storage could not only result in practitioners observing discrepancies in their treatment regimes, but also account for some study discrepancies, said Prof Bullimore. “When you look at the data from the LAMP study, they weren’t getting the same amount of dilation or loss of accommodation as they did in ATOM2. So the question is, what are we getting in practice when we order atropine from a compounding pharmacy?”
Prof Bullimore suggested testing compounded low-dose atropine potency by treating the patient in one eye, using the other as a control and following up after four weeks. “The control eye means it’s easier to assess dilation without relying on recreating the same measurement conditions a month later. If we’re not getting robust dilation, maybe our atropine is not what we think it is, or the drop isn’t being used.” This method means you can also be a bit more aggressive with treatment and try 0.025% or 0.05%, knowing the patient has an untreated eye, so it won’t disrupt their schoolwork, he said.
Potential solutions
To circumvent the pH-compounding issue, alternative formulations and delivery methods are being trialled. In October 2023, Vyluma and Nevakar announced results of the phase 3 CHAMP clinical study on the preservative-free 0.01% atropine drop, NVK002. Vyluma founder and CEO Dr Navneet Puri acknowledged in a subsequent Review of Myopia Management interview that low pH in ophthalmic products can lead to poor adherence due to patients’ eye discomfort. He also said many compounding pharmacies may be poorly equipped to formulate high-quality, low-dose atropine consistently. “For this reason, compounded ophthalmic formulations may have an inconsistent shelf life, dosing, efficacy and eye comfort, leading to a negative patient experience and potential treatment failure. Preservative-free formulations of low-dose atropine can avoid the toxicities and side effects associated with prolonged exposure to BAK (benzalkonium chloride) and other preservatives.”
US pharmaceutical company Eyenovia’s Optejet dispenser, designed to administer about a fifth of the volume of a traditional eye drop via a mist, may also address the compounding issue, said Prof Bullimore, allowing a lower pH but with less of a stinging sensation than a big drop. Optejet also has Bluetooth capability to monitor patient adherence.


Eyenovia’s Optejet dispenser reportedly delivers 6-8μL, consistent with the eye’s tear film capacity, in about 80 milliseconds to beat the blink reflex
Other options being assessed include Santen and Sydnexis’ SYD-101 atropine drop, which uses deuterated (‘heavy’) water as a solvent to slow the hydrolysis of atropine while maintaining a comfortable, more neutral pH for the patient. Having recruited 840 patients between the ages of three and 14, two arms of the company’s three-year phase 3 Staar trial are due for completion soon, with US and European subjects being trialled with 0.01% and 0.03% atropine doses, and a phase 3 Chinese study planned. Meanwhile, in early 2023, US company Cloudbreak Pharma completed a phase 1/2 study in Brisbane to evaluate the safety, tolerability and pharmacodynamics of CBT-009, a non-aqueous, preservative-free atropine eye drop, in 84 healthy volunteers, and has subsequently gained FDA approval for a phase 3 clinical trial in the US.
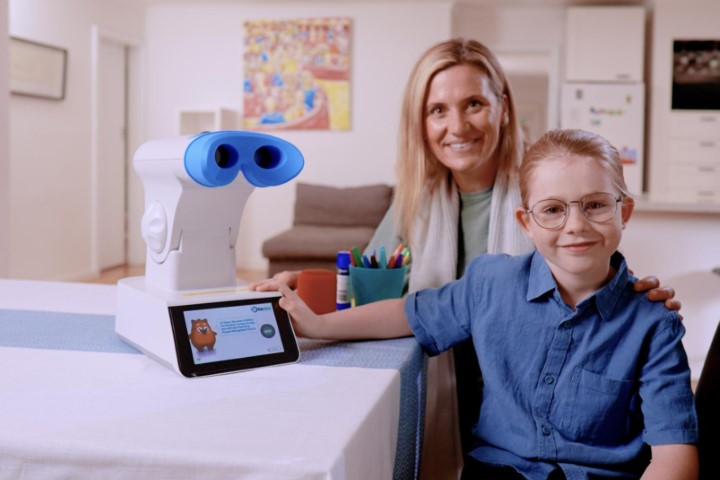
Regardless of how it’s formulated and delivered, atropine might not have the last word in the war on myopia, however, said Petty. “The new kid on the block is the red-light therapy from Eyerising which is an alternative to atropine as a myopia control-and-treatment combo.” Petty has recently included Eyerising in his own practice tool kit and said it will possibly be easier and more effective than atropine drops. We’ll just have to wait and see!