Paediatrics for dispensing opticians – part 1: the growing eye
The management of myopia is one of the key elements of clinical practice and represents one of the dominant topics for practitioner development in the future. For the practicing dispensing optician (DO), an understanding of the growth of the human visual system is one of the underlying elements of that development, with a knowledge of emmetropisation vital to meaningful engagement in the management of young eyes.
It may not be immediately apparent to the DO that there is not a well-defined, single, predictable pathway for the development of an emmetropic eye. Some relationships, such as axial length and refractive error, as well as relationships (or ratios) that inform our understanding of the outcomes of these growth processes are well known. Unfortunately, the process of emmetropisation is highly individual and reliant on a range of biometric, genetic, refractive and environment factors and as such is not yet fully understood.
At birth, the prevalence of refractive error is overwhelmingly biased towards hyperopia, usually in the order of +2.00D. Any deviation from this state at birth is often considered an indicator of congenital refractive error, or due to factors other than post-birth developmental influences.
In the first years of life the child’s refractive error follows a reasonably predictable pathway. After an initial phase of relatively rapid change (up to around two years of age), the residual power is expected to taper gradually until the child ideally has no refractive error, via the process of emmetropisation. Theories for emmetropisation often centre around the relationship between a visual stimulus (such as blur), and the physiological response of the eye to attempt to modulate refractive error via the growth of the eye overall. In short, blur caused by refractive error stimulates a growth response whereby the eye ideally ‘grows into’ the refractive error, resulting in the refractive power of the eye being well matched with the overall axial length.
This interplay is sensitive to external influences, so any intervention is considered part of a holistic process, including management of a range of external factors that can impact visual development. Beyond emmetropisation, several other factors can influence a child’s refractive outcome. These include the lenses used in the correction of refractive error, with improper use of single-vision lenses being problematic. Since parental refractive error can also be a key indicator of issues for a child, optometrists will often look to the parents and the patient’s ethnicity, to gain insight into potential outcomes.
Why axial length?
By now, axial length is a familiar term for most of us, but why do we place so much importance on it? Research suggests corneal growth is relatively static by around three years of age, indicating that other biometric elements are responsible for the development of refractive error, more specifically myopia. There is a well-established relationship between axial length and refractive error – as the axial length increases, we find the refractive error becomes more ‘minus’. Conversely, we can expect shorter eyes to tend towards hyperopia, with the magnitude of refractive error linked to the length of the eye. Growth will therefore tend to yield myopic results instead of hyperopic, which is in line with our observations in practice. This extra length in the eye is also the source of many of the long-term ocular health issues for high myopes, such as glaucoma, retinal detachment and myopic maculopathy, hence the urgency with which we treat this condition.
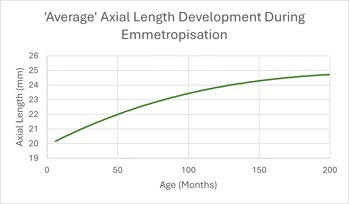 Fig 1. Axial length growth (illustrative only)
Fig 1. Axial length growth (illustrative only)
While graphs showing axial length growth often show smooth curves (Fig 1), it is also worth examining the rate of change, as shown in Fig 2. This helps us understand the periods in development where the greatest rates of change, and therefore growth, are occurring. They can also be useful for showing when a patient is experiencing a growth acceleration that does not conform to expected patterns. Axial length, however, is a lag indicator rather than a predictive measure, making research into the factors driving emmetropisation an important endeavour to facilitate interventions.
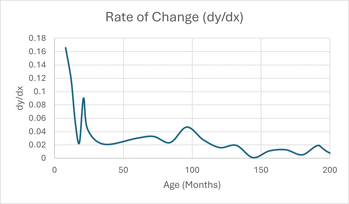 Fig 2. Rate of change (illustrative only)
Fig 2. Rate of change (illustrative only)
So where does this leave the DO? The collection of data and the management of the patient interaction with the clinic is vital and one that is difficult to monitor in the short periods available to the optometrist. Understanding where the risk points exist for the patient, as well as why we are collecting data such as biometry and patient histories, gives context to the tasks. This, in turn, is linked to better quality data and better patient outcomes.
This is the first of two articles on this topic, with the second expected later this year. Both follow on from the article ‘Myopia management applications’ published in March.

Grant Hannaford is a senior lecturer at the School of Optometry and Vision Science UNSW, the past-chair of the NSW Optical Dispensers Education Trust and the past-vice president of ADOA (NSW). A co-founder and director of the Academy of Advanced Ophthalmic Optics, he co-owns Hannaford Eyewear and was 2022’s Silmo IOA International Optician of the Year. Australia’s first qualified spectacle lens designer, Hannaford is a doctoral candidate at Aston University, UK, where he’s researching emmetropisation and ocular biometric development in children.