Paediatrics for dispensing opticians: Part 2 – integrating the dispenser
In our July 2024 article we outlined some of the concepts surrounding monitoring the juvenile eye’s growth to provide background for describing interventions undertaken by optometry.
The outcomes for suboptimal emmetropisation in children extend beyond the presence of residual refractive error into adulthood. It is well established that myopisation carries a host of elevated risks for conditions including myopic maculopathy, glaucoma, retinal detachment and cataract. Less prominent in the professional dialogue are the associated issues arising from hyperopia and astigmatism such as amblyopia, binocular vision disfunctions and glaucoma. Dispensing opticians (DOs) play a key role in ensuring interventions are well implemented and patient compliance is maintained.
Selection of intervention
Common queries on optical discussion forums include ‘What is the best lens?’ or ‘What is the best lens for myopia control?’. While there is no shortage of response to these threads, it is almost always the case that any advice is given without the full case data. For example, in myopia management, clinical results such as binocular vision performance will be the difference between lens selections, so while the optician may want to give a newer solution such as a defocus incorporated multiple segments (DIMS) lens, it may not be appropriate. This is often a source of disappointment for parents who may associate the latest lens technology with enhanced success, when a prism control bifocal may actually be the most appropriate response. The appearance or cosmesis of a lens is of obvious importance for children; however, the clinical efficacy of the selected pathway should always be the primary consideration.
Fitting considerations
Optically imposed astigmatism has been observed in studies to influence the emmetropisation pathway1-3. While the magnitude of imposed astigmatism in research is significant, it is also understood that poor placement of even single-vision lenses can induce optically imposed oblique astigmatism. The magnitude of these errors is smaller than that used in research but may still operate on a scale that can influence refractive developmental pathways. For example, a +3.00DS lens fit on datum with no consideration for tilt, wrap or back vertex distance will induce an effective power of approximately +3.25/-0.43 x 167. While position-of-wear compensations readily overcome such errors, they can also be relatively easily addressed through appropriate application of the centre of rotation fitting principles4.
Prism represents another simple, yet often overlooked, pathway for improvements in the efficacy of prescribed interventions for children’s visual development. Optometry will often use prism in carefully defined applications, particularly in the presence of binocular vision defects, to influence development. While the applications for addressing tropia and avoidance of amblyopia are perhaps the most common areas understood by DOs, the application in myopia management is also as important for the selection of appropriate lens treatments. Of note is the disconnect that can develop between the care taken when prescribing prism in the consultation and the somewhat looser attitude taken with regard to fitting of the optical appliance. A prescription with prism usually garners more attention for fitting accuracy that one without. Yet a prescription with no prism defined actually does have a prism requirement specified – namely a demand that zero prism is present at the eye in the final appliance. With this in mind it is strongly encouraged that every patient’s monocular measurements are taken for every parameter. Simple calculations show that, in our earlier example, datum fittings can result in over 1.50 Δ of yoked prism and clinically significant amounts of differential prism can arise in the presence of even relatively small power differences between eyes. This is exacerbated by horizontal (pupillary distance) fitting errors, which can be easily overcome through application of asymmetrical values wherever they arise.
A simple process flow (Fig 1) can be useful for practitioners when working with paediatric dispensing:
1. Rx – treat each element of the prescription as immutable. Even the absence of a value (such as no cylinder or prism) should be treated as that value equalling zero
2. Lens selection – primarily a clinical consideration, with cosmetic concerns coming second in every instance
3. Fitting – all parameters matter. We understand children will be relatively inconsistent with the placement of the frames on their face. This makes the accurate fitting of the lenses more important as we need to minimise the impact of this movement as much as possible to reduce the influence of optically imposed errors due to fitting.
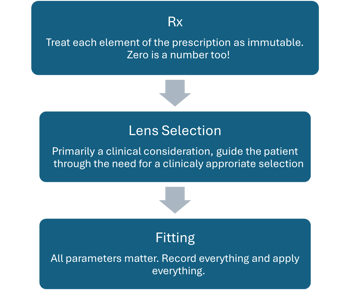
Fig 1. This simple process flow can be useful for practitioners when dealing to paediatric dispensing
Optically imposed errors pose a unique challenge in paediatric optometry, as they can disrupt emmetropisation by distorting visual input, straining the binocular system and potentially leading to eye misalignment or refractive errors. For young children, whose eyes are still in their critical stages of development, stable, clear and consistent visual input is essential for normal eye growth. Proper spectacle fitting, lens positioning and regular follow-ups are crucial in minimising induced prism, enabling children’s visual systems to develop healthily and reducing the risk of long-term visual issues. Through vigilant fitting and monitoring practices, we can ensure children receive the full benefit of their prescriptions, effectively supporting emmetropisation and overall visual development.
References
1. Kee CS, et al. Effects of optically imposed astigmatism on emmetropization in infant monkeys. Invest Ophthalmol Vis Sci, 2004. 45(6): p. 1647-59
2. Hughes AR, Mallen EA and Elliott DB. The Visual Impact of Lens-Induced Astigmatism is Linked to Habitual Axis. Optom Vis Sci, 2017. 94(2): p. 260-264
3. Zhang J, et al. Epidemiology and Burden of Astigmatism: A Systematic Literature Review. Optom Vis Sci, 2023. 100(3): p. 218-231
4. Ohlendorf A, Schaeffel F and Wahl S. Positions of the horizontal and vertical centre of rotation in eyes with different refractive errors. Ophthalmic Physiol Opt, 2022. 42(2): p. 376-383.

Grant Hannaford is a senior lecturer at the School of Optometry and Vision Science UNSW and co-owns Hannaford Eyewear. He was 2022’s Silmo IOA International Optician of the Year and is now a doctoral candidate at Aston University, UK, researching emmetropisation and ocular biometric development in children.
























