Pathologic myopic and myopic choroidal neovascularisation
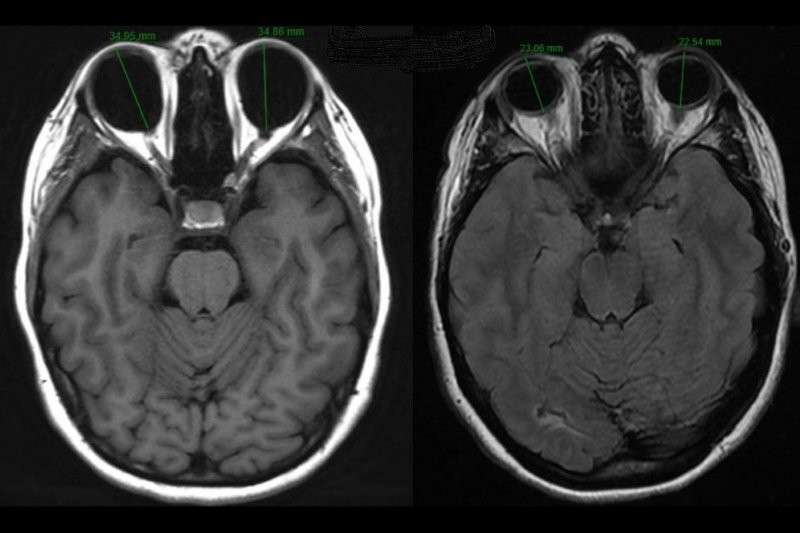
High myopia is commonly defined as a refractive error of at least -6 dioptres and/or an axial length of greater than 26.5mm. The term pathological myopia, interchangeably used with myopic maculopathy or degenerative myopia, describes high axial myopia and is associated with degenerative changes in the retina. It is thought to affect 3% of the global population1. Ethnic origin seems to influence the likelihood of developing pathological myopia. The prevalence is higher in Asian populations and lower in African and Pacific island groups2.
Clinical Features of pathological myopia
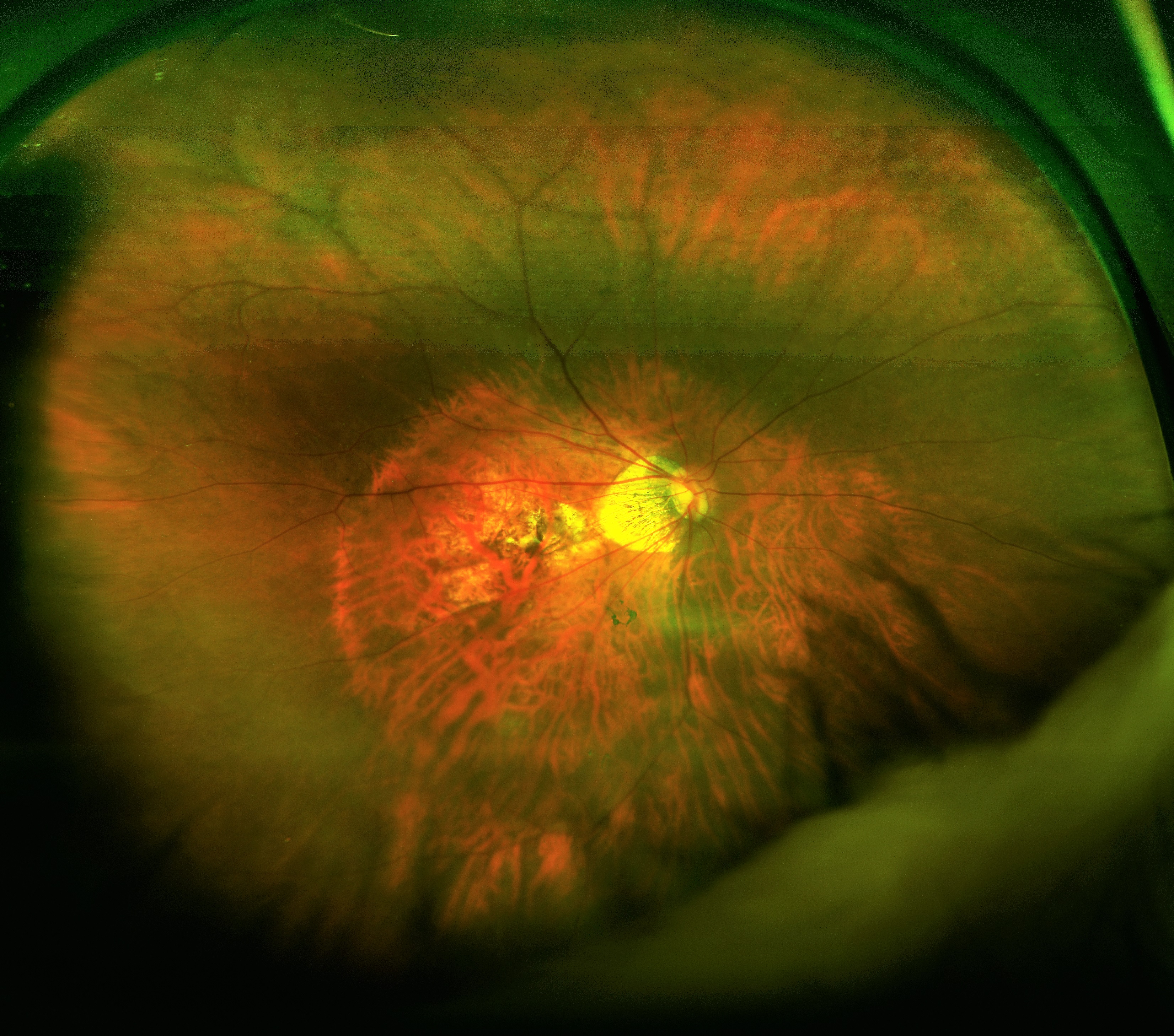
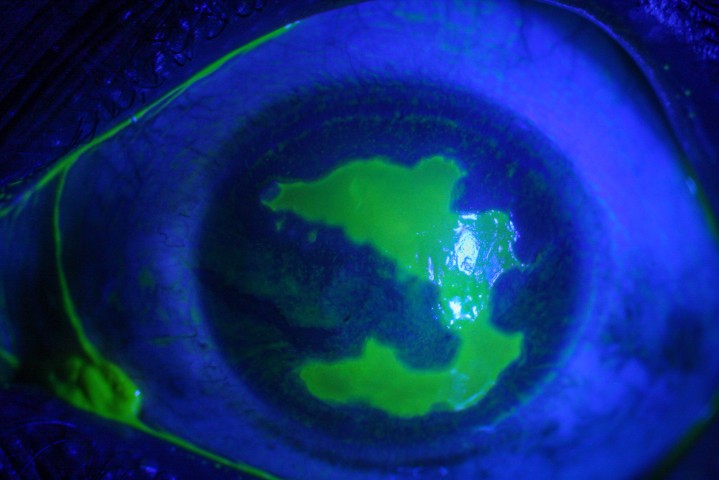
Figure 1: Widefield optos image of myopic fundus demonstrating a tessallated fundus, tilted optic disc with a myopic cone and macula atrophy. The outline of a poterior staphyloma is also visible
Posterior pole abnormalities typically found in pathological myopia include:
- Tessellated fundus - where depigmentation due to RPE atrophy leads to variation in the visibility of the large choroidal vessels throughout the fundus
- Tilted optic disc with myopic cone – this is in part due to the peri papillary scleral expansion which results in a hypo-pigmented myopic crescent or a myopic cone is seen where sclera is directly visible. The tilted appearance of the optic disc is characterised by temporal flattening of the disc
- Posterior staphylomas - an outward outpouching of all coats of the posterior pole and considered pathognomonic for pathologic myopia. The incidence increases with age and is further associated with the development of myopic maculopathy
- Lacquer cracks – these are breaks in the Bruch's membrane at the macula in highly myopic eyes usually associated with a posterior staphyloma. These appear as multiple yellowish-white irregular lines, usually horizontally oriented, and coursing the posterior pole
- Foster Fuch’s spots- are areas of RPE proliferation following choroidal haemorrhage. They follow high myopia-related degeneration and neovascularisation. Clinically they appear raised and pigmented, but can occasionally appear yellow or greenish
- Myopic choroidal neovascularisation (CNV) – this is the most common cause of central vision loss in pathologic myopia and will be discussed in greater detail below. On examination, it typically appears as a small, flat, greyish membrane located subfoveal, but can be juxtafoveal, extrafoveal or peripapillary
- Myopic macula retinoschisis and myopic macula hole - Myopic macular retinoschisis or myopic foveoschisis describes a schisis-like thickening of neurosensory retina into a thicker inner layer and a thinner outer layer at the macula in highly myopic eyes with a posterior staphyloma.
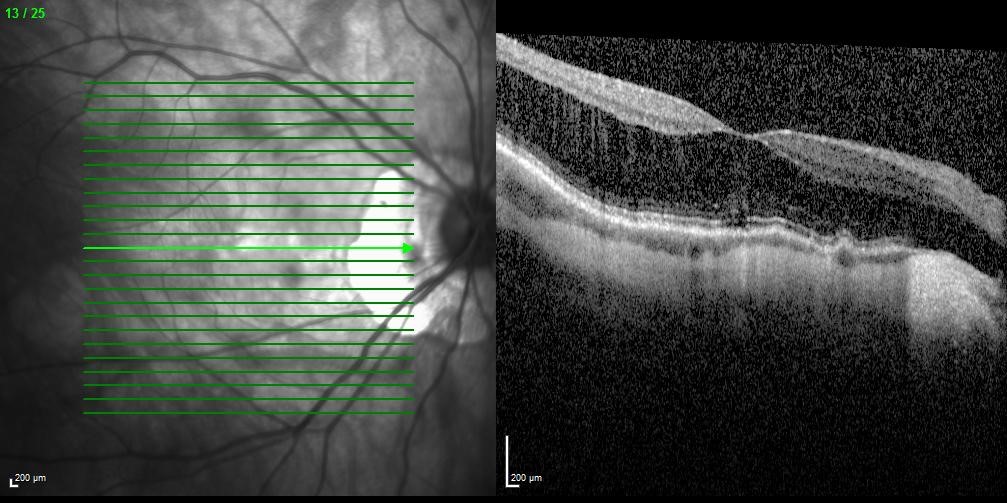
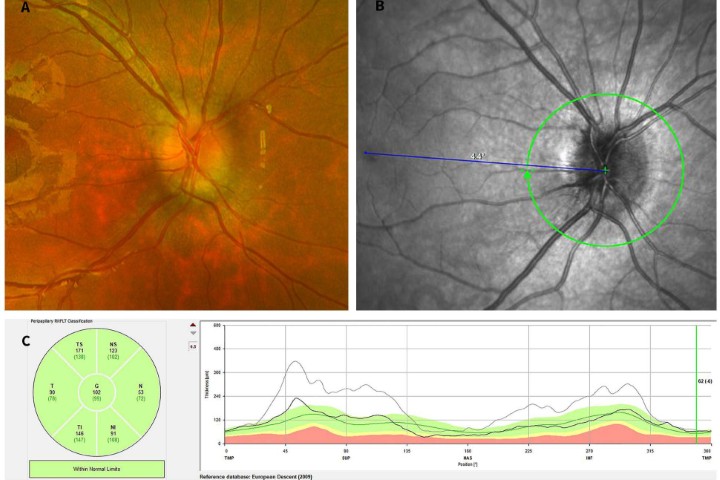
Figure 2: Myopic macula schisis with a thicker inner layer and a thinner outer layer at the macula
Classification and progression of pathologic myopia
Various classification systems have been proposed for pathologic myopia over the last 30 years, including long-term progression studies of myopic maculopathy to define a number of stages3,4. Progression was variable, but noted to be the least with a tessellated fundus alone. Functional defects were much more common with the presence of a CNV, lacquer cracks or patchy atrophy. Most recently a photographic classification and grading system (Table 1) has been proposed for myopic maculopathy with five main classes and three “plus lesions”, which can co-exist across categories. With the higher categories, there is a higher risk of developing myopic CNV. Pathologic myopia was defined as worse than category two, ie. with the presence of chorioretinal atrophy5. Posterior staphyloma is described separately as it is not limited to the macula region.
|
International classification for pathologic myopic maculopathy |
|||
|
Category |
0 |
No macula lesions |
“Plus lesion” |
|
1 |
Tessellated fundus |
|
|
|
2 |
Diffuse chorioretinal atrophy |
|
|
|
3 |
Patchy chorioretinal atrophy |
|
|
|
4 |
Macula atrophy |
||
Table 1: International classification for pathologic myopic maculopathy
Myopic CNV
Myopic CNV represents one of the most serious complications of pathologic myopia, with a prevalence of 5-11% in pathologic myopia, although this is thought to be an underestimation1. Furthermore, 35% of these patients will develop bilateral disease in eight years6.
The pathogenesis is not fully understood, nor is the relationship between the degree of myopia, the development and progression of pathologic myopia and myopic CNV.
Ocular risk factors include patchy atrophy and lacquer cracks, choroidal thinning at the posterior pole and presence of choroidal filling delay7. The natural history is quite varied and visual prognosis can be poor even with treatment. Patients present with sudden central visual loss at the time of the CNV, accompanied by scotoma or metamorphopsia. This is often quickly stabilised, however there can be a progressive deterioration over time predominantly due to the development of patchy atrophy. It has also been shown that the long-term visual prognosis is influenced by age at onset with patients >40 years having a worse prognosis8.
Clinical examination demonstrates a small, flat, greyish subretinal membrane, often with a hyper-pigmented border and, as mentioned, most are subfoveal. Compared to membranes associated with age-related macula degeneration, subretinal fluid, haemorrhage and exudate are less common.
Spectral domain OCT (SD-OCT) is extremely useful for evaluating myopic CNV as well as associated features like posterior staphyloma, retinoschisis, thinned choroid, macula atrophy or macula hole formation. On SD-OCT, myopic CNV appears as a type 2 (subretinal, as opposed to sub-RPE) membrane and is associated with a very thin choroid, evident most using the enhanced depth imaging protocol on the OCT. In fact, choroidal thinning is more prominent in eyes with myopic CNV than myopic eyes without CNV9. On fluorescein angiogram, 90% of myopic CNV is hyper fluorescence in the early phase, followed my dye leakage in the late phase. Its particular use lies in assessing activity and recurrences.
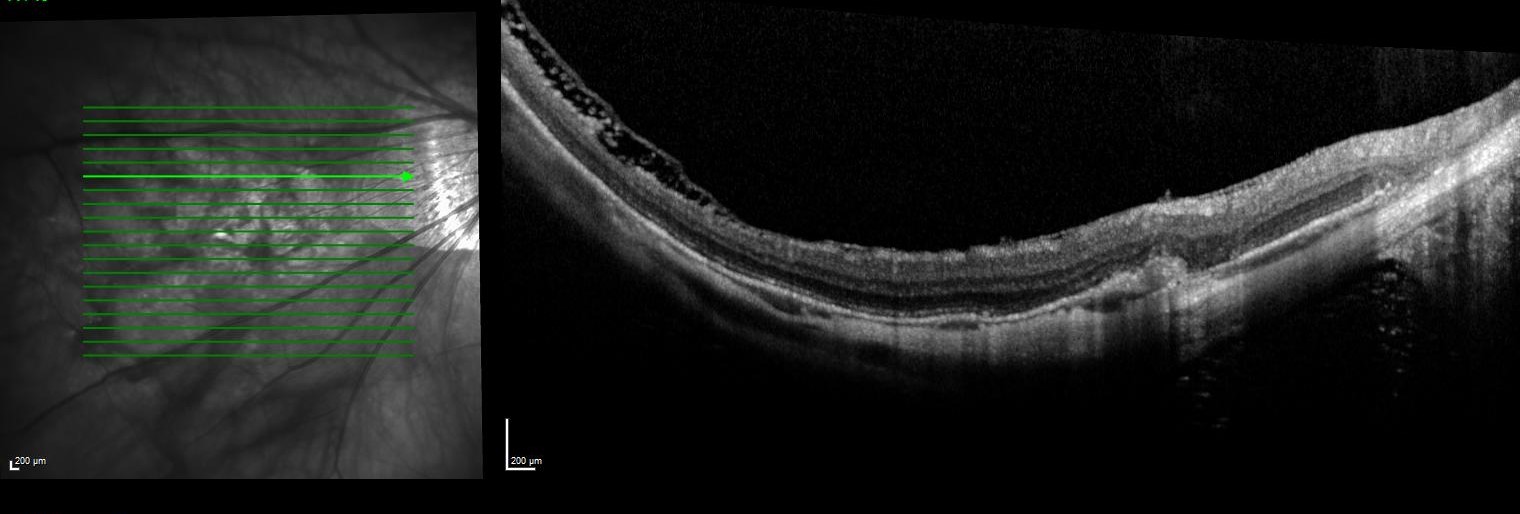
Figure 3: SD OCT of the the right eye shown in figure one demonstrating a thin choroid, extrafoveal retinoschsis and a scarred myopic CNV
Treatment of myopic CNV
Anti-VEGF injections have become the mainstay of treatment for myopic CNV. Prior to these, various approaches were explored including macula relocation surgery, thermal laser photocoagulation, corticosteroid injections and photodynamic therapy. A recent systematic review and meta-analysis of this body of evidence, has concluded that anti-VEGF therapy could be considered as first line therapy10. All four anti-VEGF injections on the market have been assessed (Bevacizumab, Ranibizumab, Aflibercept and Pegaptanib). In New Zealand, Bevacizumab remains the initial treatment choice.
After diagnosis of myopic CNV, treatment should begin without delay, and ideally within one week. Generally a 1+PRN regime is used, where a single injection is followed by an as-needed re-injection plan. The aim is to make the CNV inactive, with improvement of visual acuity and resolution of haemorrhage as secondary aims in the first six months. Close monthly monitoring is needed with regular assessments and OCT scans. The lesions typically respond rapidly to treatment and CNV recurrence is quite low with anti-VEGF therapy. The decision to re-treat is guided by new or persistent visual symptoms, or signs of activity on OCT like intra-retinal cystic changes or leakage on fluorescein angiogram.
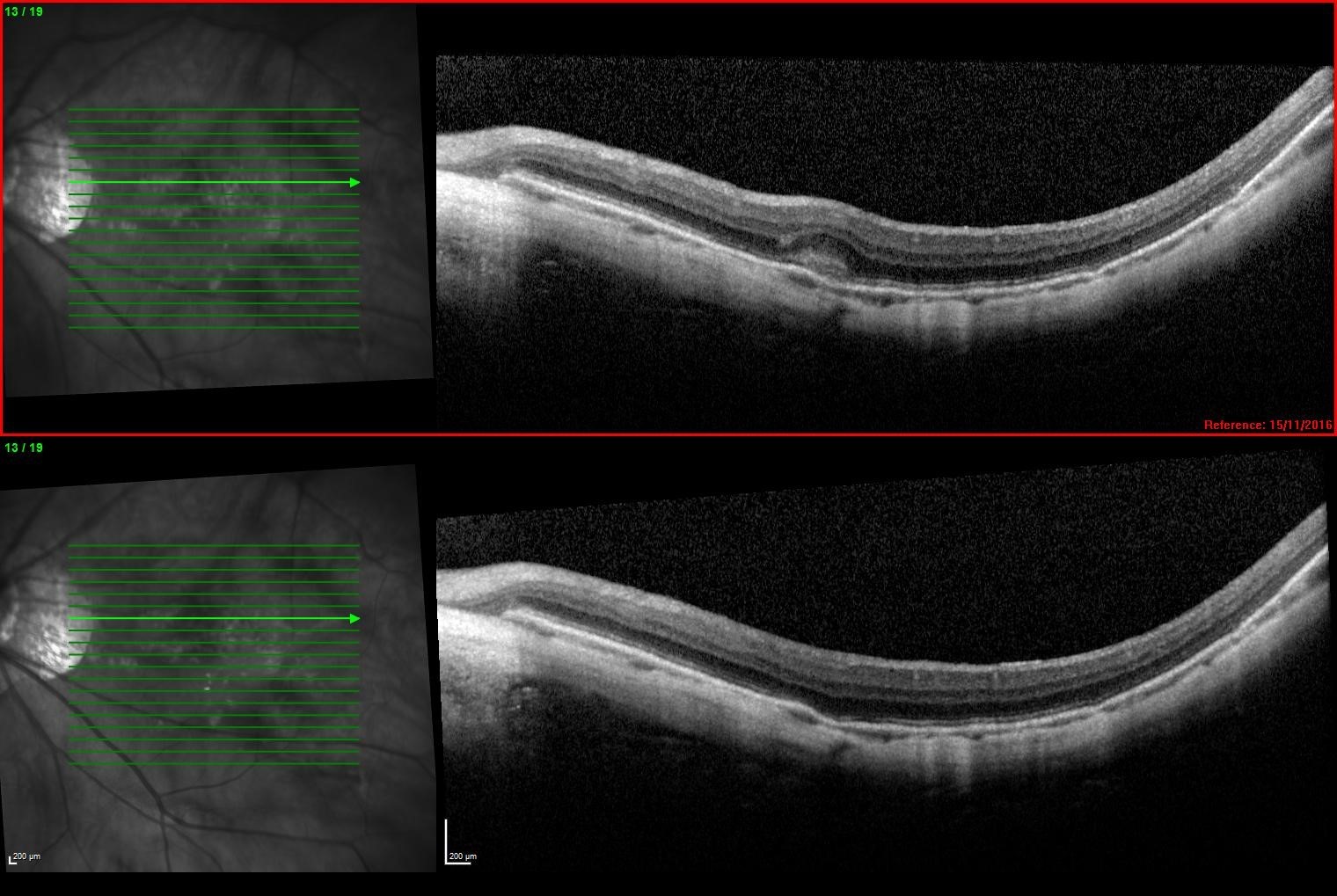
Figure 4: SD OCT with a newly diagnosed myopic CNV (above) and the same CNV 1 month following a single intravitreal Bevacizumab injection (below)
Summary
The prevalence of myopia and its complications, such as pathologic myopia and myopic CNV, pose a significant social and economic burden as it frequently affects the younger, working-age population. High-risk patients need to be identified and educated. Highly-myopic patients who present with sudden loss of vision need to be evaluated for myopic CNV and treated with anti-VEGF as soon as possible.
References
- Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Wong TY, Ferreira A, Hughes R, et al. 2014, Am J Ophthalmol, pp. 157(1) 9-25.
- Prevalence of myopia in adults: implications for refractive surgeons. McCarty CA, Livingston PM, Taylor HR et al. 1997, J Refract Surg.
- Natural history of choroidal neovascularisation in degenerative myopia. Avila MP, Weiter JJ et al. 1984, Ophthalmology, pp. 91:1573-1581.
- Long term pattern of progression of myopic maculopathy- a natural history study. Hayashi K, Ohno-Matsui K et al. 8:1595-1611, s.l. : Ophthalmology, 2010, Ophthalmology, Vol. 117, pp. 117:1595-1611.
- International photographic classification and grading system for myopic maculopathy. Ohno-Matsuri K, Kawasaki R et al. 2015, American Journal of Ophthalmology, pp. 159:877-883.
- Patchy atrophy and lacquer cracks predispose to development choroidal neovascularisation in pathological myopia. Ohno-Matsui K, Yoshida T, Futugami S et al. 2003, British Journal of Ophthalmology, pp. 87:570-573.
- Myopic maculopathy: a review. Silva, R. 2012, Ophthalmologica, pp. 228(4)197-213.
- Long term visual prognosis of choroidal neovascularisation in high myopia: a comparison between age groups. Yoshida T, Ohno-Matsui K et al. 2002, Ophthalmology, pp. 109:712-719.
- Ocular risk factors for choroidal neovascularisation in pathologic myopia . Ikuno, Y, Jo Y et al. 2010, Investigative Ophthalmology and Visual Science, pp. 51:3721-3725.
- Intravitreal anti-vascular endothelial growth factor for choroidal neovascularisation secondary to pathologic myopia: systemic review and meta-analysis . Wang E, Chen Y. 2013, Retina, pp. 33:1375-1392.
- Prevalence and progression of myopic retinopathy in an older population. . Vongphanit J, Mitchell P, Wang JJ. 2002, Ophthalmology , pp. 109;707-714.
- Proposed classification of posterior staphylomas based on analyses of eye shape by three-dimensional magnetic resonance imaging and wide-field fundus imaging. Ohno-Matsui, K et al. 2014, Ophthalmology, pp. 121:1798–809.
About the author
Dr Narme Deva, MBChB MD FRANZCO, is a consultant ophthalmologist and sub-specialist in medical retina and uveitis. She has a Doctorate in Medicine from the University of Auckland and fellowship training from the prestigious Moorfields Eye Hospital, London. Dr Deva holds a consultant post at Greenlane Clinical Centre and at Retina Specialists in Parnell.