Pioneering procedure for AMD in NZ
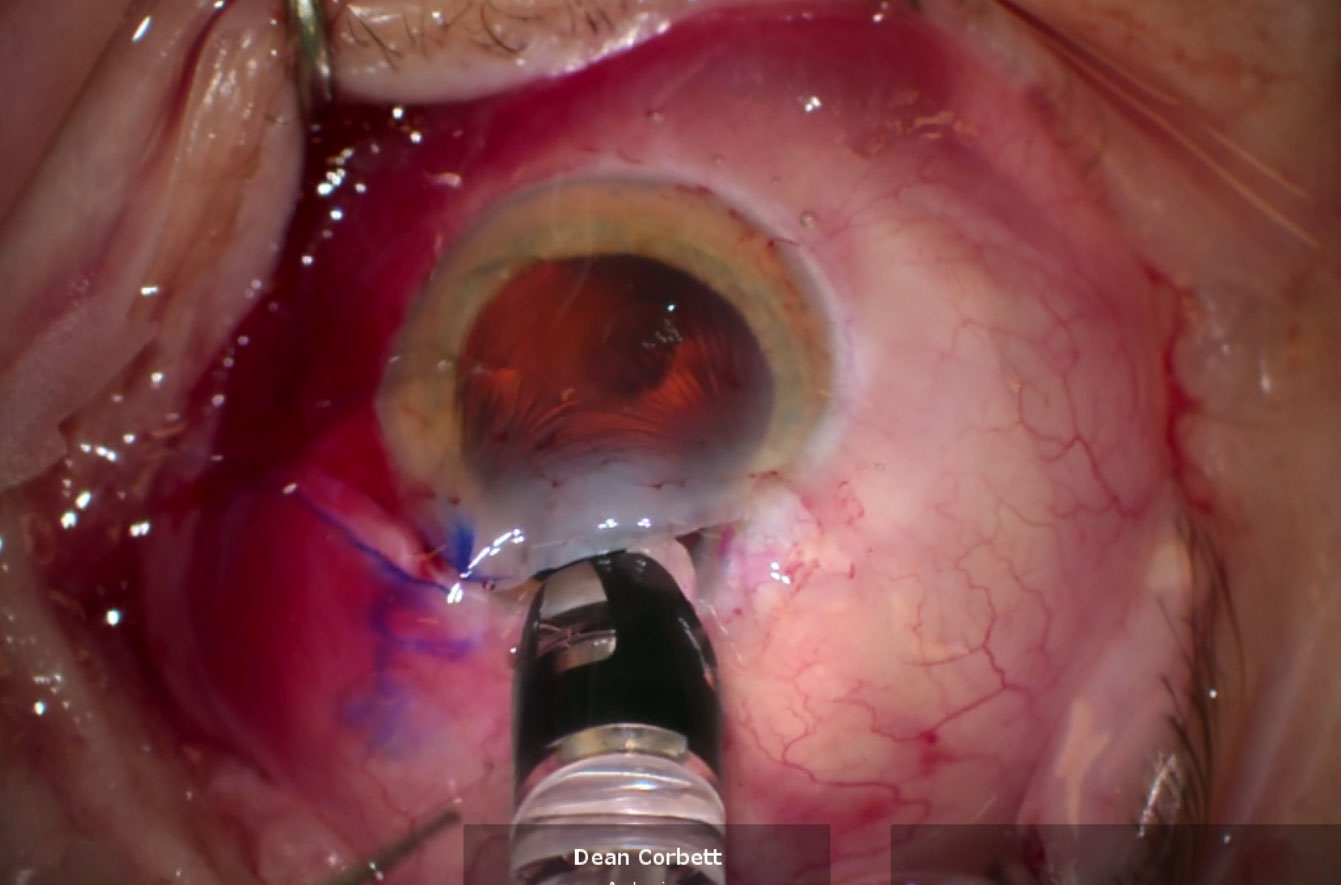
In a New Zealand first, a patient with age-related macular degeneration (AMD) has undergone a pioneering procedure with the Samsara SING IMT (smaller-incision new-generation implantable miniature telescope).
Dr Dean Corbett, who performed the operation at Auckland Eye, removed the patient’s cataract before establishing the patient’s eye was unfortunately too small to continue with the implant. It’s impossible to know exactly what you’ll find until you’ve opened the eye, said Dr Corbett, noting that patient suitability is critical to procedures such as this.
“The concept of IOT (intraocular telescopes) has been around for a while,” said Dr Corbett. “As always with these things, it’s difficult to know exactly how it will pan out until you’ve got your hands on it yourself, because there’s a lot of hype around it that’s not necessarily 100% representative of the true outcomes.”
The SING IMT, inspired by the Galilean telescope, consists of an optical component, like a miniature telescope (about 3.6mm diameter) and the haptics, like wings or petals, which are used to keep the telescope supported and centralised. The ‘petals’ create an overall diameter of 10mm.
The device provides about 2.7x magnification, or about three-to-four lines on a vision chart, said Dr Corbett, and is placed in one eye, leaving the untreated eye for peripheral vision. The technology reduces the impact of central scotoma (the characteristic ‘blind spot’ in the middle of an AMD patient’s vision), so should help patients with reading, knitting, gardening and identifying human faces. “To restore someone’s ability to interact with their environment, to be able to read again, to be able to recognise faces, to be more independent – what’s that worth?” said Dr Corbett.
Communicating risks and benefits
Dr Corbett is accustomed to performing firsts, having done “tens of thousands” of lens implants. “So my technique’s been refined,” he said. It’s about engaging the patient as a partner in the process rather than a guinea pig, he said. “There always has to be a first in any procedure or with any medication and it’s really just a lot of discussion, using terms people understand and trying to put the risk profile and the benefit profile into context as best you can. If you’ve got confidence with the surgery, then you can feel confident engaging the patient and allaying their fears… It’s about being 100% honest upfront.”

Dr Dean Corbett
The procedure was expected to take about 20 minutes, as opposed to about five minutes for a regular lens implant, explained Dr Corbett, adding that nearly all AMD patients will also have cataracts to deal with. The main risks are around the procedure and recovery, he said. “It’s a bigger wound (than a regular intraocular implant), since it’s a big device going into the eye, so everything’s got to be meticulous from a surgical point of view.”
Recovery is also paramount because the device creates a whole new visual experience for the patient, said Dr Corbett. “You’re generating something for the brain to interpret which is different, so that’s part of the variability of outcome, the process of learning… how it’s brought together in the brain, so that somebody can get the best benefits out of the product.”
From follow-up at one month, the patient will have to undertake a very intensive optometric training regime to optimise visual adaptation to their new method of seeing, he said.
Patients with significant macular pathology which is not rapidly progressive and who have not yet had lens replacement surgery are the most suitable candidates for SING IMT, said Dr Corbett. However, cost could be an issue, with the lens and procedure costing around $12,000, he said, adding that New Zealand has the lowest funding for AMD treatment in the OECD. “Southern Cross has not come on board to any degree with any lenses that have special properties.”
It’s not that it’s not an appropriate medical intervention, added Dr Corbett. “It’s just not viable from a fiscal point of view for the funders because they can’t collect enough revenue to pay for the outcome. Australia is way out front, they’re the only country I’m aware of that funds what can be called premium lenses - intraocular lenses that deliver better outcomes for people that are measurable - as opposed to just funding your standard entry-point IOL.”
The march of technology
In New Zealand, it’s estimated that more than 200,000 people over 50 years old suffer from AMD. So far three SING IMT procedures have been performed successfully in Europe and two in Australia.
The development path in ophthalmology is “pretty long and rich”, said Dr Corbett. But tech advances are gradual, incremental, he said, when asked if he’d observed a growth in developments more recently. “AI will definitely play a role in terms of outcomes… (but) it’s been steady steps, generally around a diagnostic tool or device which has opened doors to new potential. We’ve been looking for holy grails – people talk about retinal transplants and eye transplants and being able to get a flexible lens that would effectively eliminate glasses and have no side effects – but they’re all still a long way away. But along these pathways, I think we need to engage and explore the potential to make small improvements that patients may well find tremendously beneficial to their daily life.”
SING IMT is another step along the way, he said, and “unless you stick your neck out a little bit to grow outcomes” significant developments are not going to happen.