Retinal haemorrhage treatment conundrums
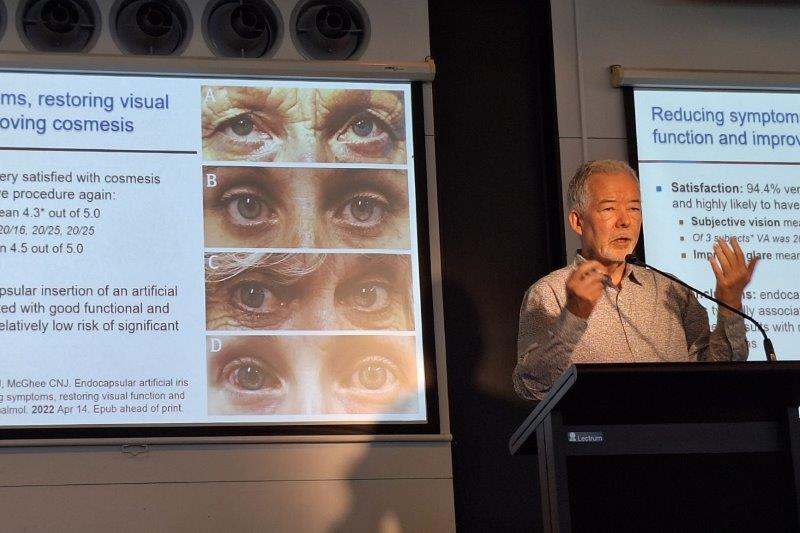
Technical issues made for an especially intimate evening at Retina Specialists’ HQ in Auckland last month, as registrars, optometrists and senior ophthalmic nurses clustered around host Dr Leo Sheck’s laptop. Undaunted by having to present his slides on such a small screen, Dr Sheck led his ‘Elevate your retina game’ seminar with a good dose of dad jokes and several keen insights drawn from cases and clinical studies.
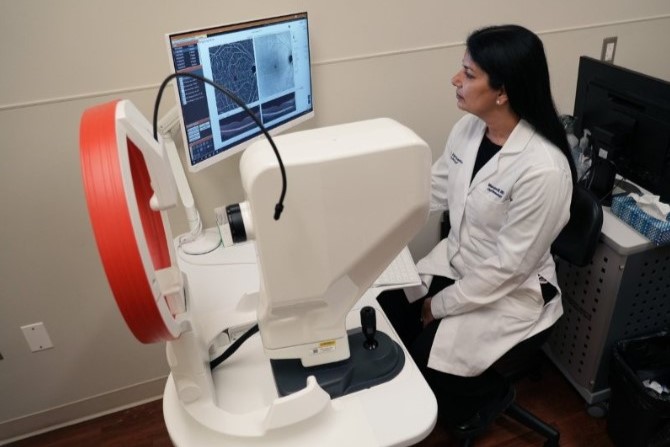
The main case of the evening centred around a fundus image of a severe submacular haemorrhage, a common clinical manifestation for optometrist-referred patients. The location, size and spread of a haemorrhage provides clues as to the underlying cause, explained Dr Sheck, the most common of which are age-related macular degeneration and its variant, polypoidal choroidal vasculopathy. Retinal haemorrhages can be treated with anti-VEGF injections and/or surgically (tPA +/- gas +/- vitrectomy). But even with a detailed history, examination and OCT imaging, the right course of treatment for patients suffering from retinal haemorrhages is not always clear, he said. “To understand what to do, one must know what happens if nothing is done.”

David Garland, Drs Michael Wang and Corina Chilibeck and Jan Chai
The seminal Anchor¹ and Marina² trials showed clearly that uncontrolled neovascular age-related macular degeneration (nAMD) leads to macular haemorrhages, with a rate of 74% for predominately classic neovascular membrane (Anchor) and 57% for minimally classic and occult membrane (Marina) over 18 months. Other studies, including the Pier studies³ and clinical reports during Covid, showed when anti-VEGF treatment was delayed, inadequately controlled neovascular activity increases the risk of macular haemorrhage, said Dr Sheck. “So it’s essential to continue the adequate suppression of neovascular activity to prevent macular haemorrhage in nAMD.”
Dr Sheck then focused on an array of other patient issues which could affect haemorrhage risk, including patients on blood thinners (doesn’t seem to be a problem as long as the neovascular membrane is adequately treated, but doubts remain) and hypertension (consider treating).
As to surgery versus anti-VEGF alone, a recent meta-analysis⁴ found both anti-VEGF and surgical treatments for submacular haemorrhages in AMD had similar visual acuity outcomes but different safety profiles. While an earlier trial⁵ showed that tPA + gas + anti-VEGF without vitrectomy gives the same visual outcome as vitrectomy + tPA + gas + antiVEGF and a subsequent study⁶ suggested intravitreal gas is not essential to achieve a good visual outcome when giving tPA and anti-VEGF for submacular haemorrhage, explained Dr Sheck.

Jennifer Lu, Alice Ku, Jason Xu and Anna Maitland
After focusing on a few more studies and cases, attendees were then put through their paces using the Slido quiz app to find out what they’d do when faced with some weird and wonderful patient OCT and fundus images. Dr Sheck also discussed New Zealand’s woeful lack of the latest drugs, including pegcetacoplan (Syfovre) and avacincaptad pegol (Izervay) for geographic atrophy. Patients can still access these privately if it’s appropriate for them to do so, which isn’t always the case, despite the hype, he said. But if a patient can benefit from something like pegcetacoplan, Retina Specialists only charges this at cost as it’s an ophthalmologist’s job to treat patients, not sell drugs, he laughed, bringing a thoroughly enjoyable evening to a close.
References
- Brown DM, Michels M, Kaiser PK, Heier JS, Sy JP, Ianchulev T; ANCHOR Study Group. Ranibizumab versus verteporfin photodynamic therapy for nAMD: two-year results of the ANCHOR study. Ophthalmology. 2009 Jan;116(1):57-65.e5
- Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY; MARINA Study Group. Ranibizumab for nAMD. N Engl J Med. 2006 Oct 5;355(14):1419-31Regillo CD, Brown DM, Abraham P, Yue H, Ianchulev T, Schneider S, Shams N. Randomized, double-masked, sham-controlled trial of ranibizumab for nAMD: PIER Study year 1. Am J Ophthalmol. 2008 Feb;145(2):239-248.
- Abraham P, Yue H, Wilson L. Randomized, double-masked, sham-controlled trial of ranibizumab for nAMD: PIER study year 2. Am J Ophthalmol. 2010 Sep;150(3):315-324.e1
- Shaheen A, Mehra D, Ghalibafan S, Patel S, Buali F, Panneerselvam S, Perez N, Hoyek S, Flynn HW Jr, Patel N, Yannuzzi NA. Efficacy and aafety of anti-VEGF injections and surgery for AMD-related submacular hemorrhage: a systematic review and meta-analysis. Ophthalmol Retina. 2025 Jan;9(1):4-12
- Gabrielle PH, Delyfer MN, Glacet-Bernard A, Conart JB, Uzzan J, Kodjikian L, Arndt C, Tadayoni R, Soudry-Faure A, Creuzot Garcher CP. Surgery, tissue plasminogen activator, antiangiogenic agents and AMD study: a randomized controlled trial for submacular hemorrhage secondary to AMD. Ophthalmology. 2023 Sep;130(9):947-957
- Murphy GSP, Saleh A, Ayis S, Cheema MR, Mehta A, Steel DH, Membrey L, Costen M, Jackson TL. Tissue plasminogen activator or perfluoropropane for submacular hemorrhage in AMD: a factorial randomized clinical trial. JAMA Ophthalmol. 2024 Dec 1;142(12):1157-1164