Shedding light on a novel microbial keratitis treatment strategy
Microbial keratitis (MK) is an acute and potentially visually devastating infection of the cornea caused by bacteria, fungi, amoebae and viruses. The infection is relatively rare in developed countries but remains a major cause of permanent blindness in low-income countries. Risk factors are well-defined and include contact lens wear, ocular surface disease, ocular surgery, low immunity, diabetes and ocular trauma.
Typically, the initial treatment for MK is broad-spectrum antibiotics, which aim to cover a wide range of bacteria, also called empiric treatment. The cornea is first debrided to culture a specimen from the infection site to identify the microorganisms in the laboratory, while empiric therapy is initiated. The initial medicine (eg, antibiotics, antifungals or others) is usually selected on the basis of the appearance of the ulcer, the presenting history and associated clinical characteristics1. After laboratory culture reports are available, treatment is optimised to target the causative pathogen, usually within 24 to 48 hours. In the interim, as the infection can progress rapidly, eye drops are often instilled every 30-60 minutes to minimise the risk of corneal perforation and permanent blindness.
Severe cases often require hospitalisation to ensure timely application of antibiotic drops, and subsequent surgical intervention may also be required due to disease sequelae. Previous research has confirmed that delayed hospital presentation, delayed diagnosis due to culturing requirements, increasing antibiotic resistance and loss to follow-up, impact the outcomes of MK in New Zealand2. Furthermore, the spectrum of pathogens in MK is evolving, with more virulent and antibiotic-resistant bacteria being isolated with increasing frequency. For example, in New Zealand, corneal infections caused by virulent P. aeruginosa from 2013-2014 were estimated to be 12.5 per million cases, up from 5.4 per million during the 1999-2000 period2,3.
Over the last two decades, several antibiotics which were previously a major line of defence against MK have lost efficacy as bacteria continue to develop a variety of mechanisms to resist these drugs. Accordingly, antibiotic resistance is feared to be one of the most devastating consequences of poor visual outcomes in MK worldwide4. There have been reports of increasing difficulties in managing devastating infections that progress rapidly, causing significant tissue damage and loss of corneal transparency, even after healing1. Among hospitalised cases of MK, more than half end up with varying degrees of corneal opacity and 20% require subsequent surgical intervention5.
As a result, there has been ongoing investigation seeking alternative treatment options to effectively manage corneal infections. Light-based anti-infective technology presents an exciting possibility as it is deemed safe and effective in treating acute and chronic infections6. Corneal collagen crosslinking is a technique often carried out in MK cases which are unresponsive to conventional medical therapy. This method uses a combination of UVA (long wavelength ultraviolet) light and the chemical substrate, riboflavin, to create a photodynamic reaction in the cornea. Free oxygen radicals generated during the process kill most microorganisms. However, crosslinking is not ideal for managing MK due to its prolonged and invasive nature, which requires 30-60 mins of treatment on a de-epithelialised corneal surface.
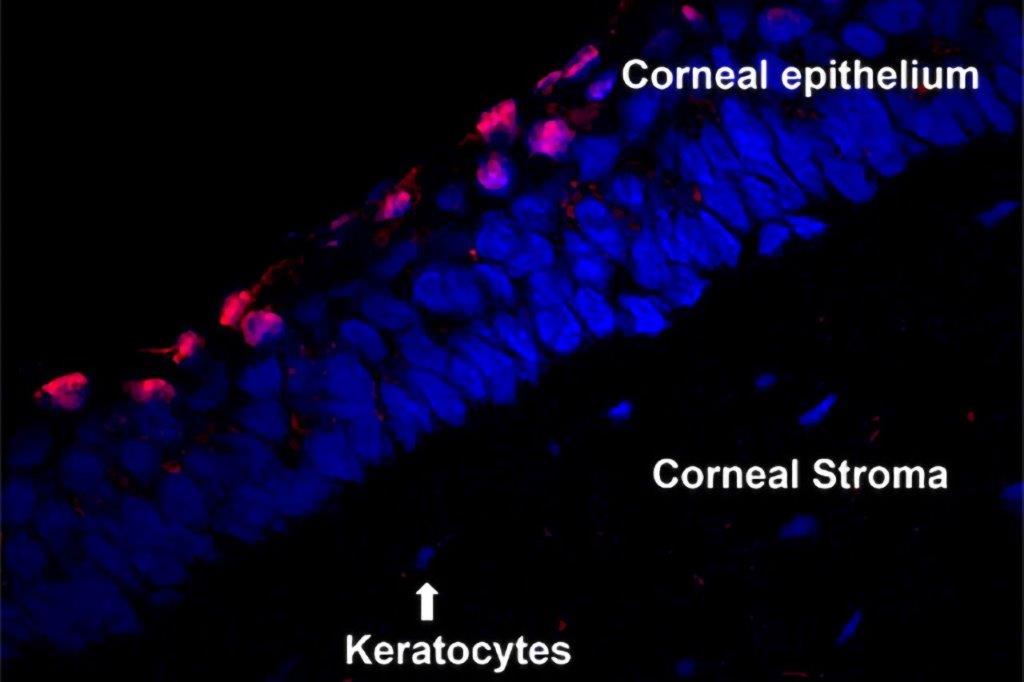
It’s encouraging, therefore, to see alternative therapeutic options on the horizon. In the Ocular Surface Laboratory at the University of Auckland, we have been investigating standalone UVC (short wavelength ultraviolet light) technology as a potential method to treat infective keratitis. UVC is efficiently absorbed by the DNA of living organisms, leading to photochemical reactions that impair DNA functions and inhibit microbial growth. Due to their simplistic cellular structure, microorganisms can be killed by much lower UVC doses – at least 20 times less – than those required to deactivate host cells (such as human corneal cells). UVC destroys most bacteria, yeast, fungi and other pathogenic microorganisms, irrespective of their antibiotic resistance profiles. For example, methicillin-resistant Staphylococcus aureus (MRSA), reported to be increasingly implicated in MK, is highly susceptible to UVC7. Our preclinical laboratory studies have established that twice-daily 15-second exposures of minimal intensity (1.93mJ/cm2) 265nm UVC can safely8 and effectively7 manage a corneal infection caused by the highly pathogenic bacterium P. aeruginosa. In an in vivo infection model developed in the laboratory, the cornea was shown to heal completely in most cases within the first 24 hours following treatment7. The treatment was also deemed safe as it did not harm corneal cells. Laboratory studies are ongoing to evaluate the impact of similar doses of UVC in managing established bacterial biofilms as these represent some of the most stubborn infections for clinicians to manage.
The future is looking ever brighter for those impacted by microbial keratitis with such groundbreaking novel anti-infective therapies in development. As a researcher, it’s rewarding to have the opportunity to delve into the basic science behind UVC, in its application as an antimicrobial agent, to understand its potential consequences and explore ways to optimise the treatment protocol to develop this technology as a cost-effective empiric treatment for microbial keratitis. Watch this space!
References
1. Austin A, Schallhorn J, Geske M, Mannis M, Lietman T, Rose-Nussbaumer J. Empirical treatment of bacterial keratitis: an international survey of corneal specialists. BMJ open ophthalmology. 2017;2(1):e000047.
2. Wong T, Ormonde S, Gamble G, McGhee C. Severe infective keratitis leading to hospital admission in New Zealand. British Journal of Ophthalmology. 2003;87(9):1103-8.
3. Marasini S, Wang M, Swift S, Dean S, Ormonde S, Gamble G, et al. Clinical and microbiological profile of Pseudomonas aeruginosa keratitis admitted to a New Zealand tertiary centre. Clinical & Experimental Ophthalmology. 2018;46(4):441-4.
4. Ting D, Ho C, Deshmukh R, Said D, Dua H. Infectious keratitis: an update on epidemiology, causative microorganisms, risk factors, and antimicrobial resistance. Eye. 2021;35(4):1084-101.
5. Marasini S. Exploring the potential of UVC in treating superficial corneal infections. PhD Thesis: ResearchSpace@ Auckland; 2019.
6. Marasini S, Zhang A, Dean S, Swift S, Craig J. Safety and efficacy of UV application for superficial infections in humans: a systematic review and meta-analysis. The Ocular Surface. 2021;21:331-44.
7. Marasini S, Dean S, Swift S, Perera J, Rupenthal I, Wang T, et al. Preclinical confirmation of UVC efficacy in treating infectious keratitis. The Ocular Surface. 2022;25:76-86.
8. Marasini S, Mugisho OO, Swift S, Read H, Rupenthal I, Dean S, et al. Effect of therapeutic UVC on corneal DNA: Safety assessment for potential keratitis treatment. The Ocular Surface. 2021;20:130-8.

Dr Sanjay Marasini is a biomedical researcher with an optometry background. His research includes clinical and scientific ocular surface evaluation in health and disease, especially in relation to microbial infections and their treatment, preferentially using novel non-pharmacological light-based technologies.