Shedding light on LLLT for dry eye disease
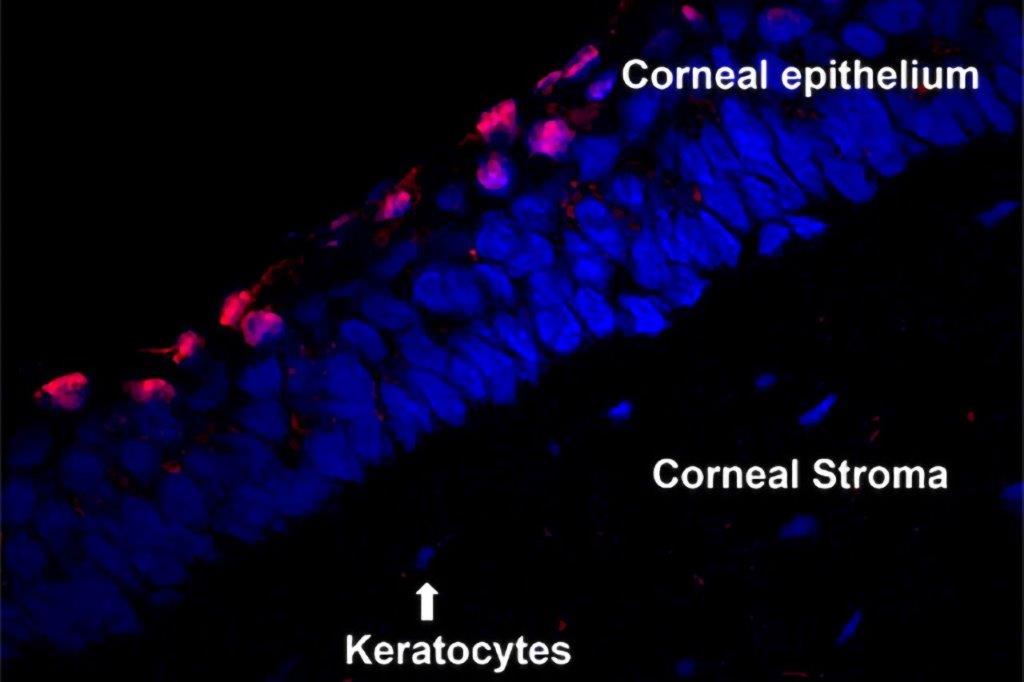
Low-level light therapy (LLLT), also known as photobiomodulation, has recently become more widely accessible as a treatment for dry eye disease (DED) in New Zealand. LLLT is believed to work by triggering conformational changes in the cellular cytochrome-c oxidase enzyme, leading to enhanced mitochondrial function, increasing adenosine triphosphate (ATP) production¹. ATP production is important as it improves cellular function of treated tissues, such as those involved in the lacrimal functional unit. Other reported therapeutic benefits from LLLT in dry eye disease include heat delivery to treatment area²-⁴, reduction of oxidative stress⁵ and reduced inflammation⁶.
Light wavelengths between 390–600nm are used to treat superficial tissue with a possible antimicrobial effect, whereas wavelengths between 630–1,000nm can reach deeper tissues⁷,⁸. Wavelengths of around 633nm are recommended in the treatment of DED. While the treatment protocol can vary, recent studies have tended to opt for 15-minute treatments, delivered with varying frequency and spacing between treatment sessions, within the manufacturer’s guidelines, tailored to suit individual patients.
A randomised controlled trial (RCT) was conducted in South Korea in 2022 comparing LLLT treatment to sham treatment in a cohort of 40 participants with DED. Treatment was provided twice a week for three weeks with follow-up measurements taken at four weeks from baseline. The active LLLT group experienced significant improvements in corneal and conjunctival staining, Schirmer test and upper lid meibography, compared with the sham treatment group. However, since the study authors did not report a significant change from baseline to week four in either group, the extent of improvement is difficult to ascertain in the LLLT group⁸.
Antwi et al published two papers in 2024 looking at the effect of a single LLLT treatment on the ocular surface and tear film² and a three-treatment protocol across three weeks³. The immediate treatment effects were a rise in eyelid temperature and tear film lipid layer thickness (TFLL), which was comparable to that achieved with the Bruder moist heat compress. The authors also reported significant improvements in non-invasive tear breakup time (NIKBUT), tear meniscus height (TMH), TFLL, OSDI, Schirmer score and meibum quality with three weekly treatments. No significant changes were reported for corneal staining or meibomian gland loss in this study. It is worth noting, however, that the three-week study did not include a sham-treatment or standard-of-care control group.
While commonly performed as an in-office treatment, Giannaccare et al explored the efficacy of at-home LLLT in 2022. In this study it was prescribed as four serial treatments for 17 participants, performed every second day. The results showed an improvement in NIKBUT, TMH and OSDI scores but, again, no control group was included in this study⁹. However, another RCT was conducted comparing LLLT and intense pulsed light (IPL) therapy across four weekly sessions for both groups, with measurements taken at baseline and at two weeks after the final treatment and at week six. The magnitude of improvement for Standard Patient Evaluation of Eye Dryness (SPEED) symptom scores was greater in the group receiving LLLT treatment than those who underwent IPL therapy. Significant improvements in TMH were seen in the LLLT group¹⁰. The improvement of TMH and Schirmer scores across multiple studies also suggest that LLLT may have the potential to improve lacrimal gland function³,⁹,¹⁰.
Treatment protocols combining LLLT and IPL have been explored. However, while several papers have reported improvements in clinical parameters11-13, RCTs comparing single LLLT or IPL treatment vs combined therapy have not been conducted to date, therefore we cannot yet conclude the benefits of combined therapy compared to single treatments.
Overall, there is a lack of recent systematic reviews on the benefits of LLLT treatment and, from this brief review of recent studies, it’s clear more randomised controlled studies are required to establish LLLT’s efficacy and optimal delivery characteristics in managing DED.
To this end, an ongoing, multicentre study is looking to explore the benefits of various LLLT treatment protocols using different wavelengths of light to further understand the mechanisms of action and help guide optimal treatment procedures. Keep an eye out for an upcoming randomised controlled study within the Ocular Surface Laboratory at the University of Auckland for which we’ll be calling upon research participants in 2025.
References
1. Garg D, Daigavane S. Photobiomodulation in Ophthalmology: A Comprehensive Review of Bench-to-Bedside Research and Clinical Integration. Cureus. 2024;16(9):e69651.
2. Antwi A, Nti AN, Ritchey ER. Thermal effect on eyelid and tear film after low-level light therapy and warm compress. Clin Exp Optom. 2024;107(3):267-73.
3. Antwi A, Schill AW, Redfern R, Ritchey ER. Effect of low-level light therapy in individuals with dry eye disease. Ophthalmic Physiol Opt. 2024;44(7):1464-71.
4. Ferraresi C, Kaippert B, Avci P, Huang Y-Y, de Sousa MVP, Bagnato VS, et al. Low-level Laser (Light) Therapy Increases Mitochondrial Membrane Potential and ATP Synthesis in C2C12 Myotubes with a Peak Response at 3-6 h. Photochemistry and photobiology. 2015;91(2):411-6.
5. Zhang C-X, Lou Y, Chi J, Bao X-L, Fan B, Li G-Y. Considerations for the Use of Photobiomodulation in the Treatment of Retinal Diseases. Biomolecules. 2022;12(12):1811.
6. Ryu JH, Park J, Kim B-Y, Kim Y, Kim NG, Shin Y-I. Photobiomodulation ameliorates inflammatory parameters in fibroblast-like synoviocytes and experimental animal models of rheumatoid arthritis. Frontiers in Immunology. 2023;14.
7. Sadick NS. Handheld LED array device in the treatment of acne vulgaris. Journal of Drugs in Dermatology: JDD. 2008;7(4):347-50.
8. Park Y, Kim H, Kim S, Cho KJ. Effect of low-level light therapy in patients with dry eye: a prospective, randomized, observer-masked trial. Sci Rep. 2022;12(1):3575.
9. Giannaccare G, Vaccaro S, Pellegrini M, Borselli M, Carnovale Scalzo G, Taloni A, et al. Serial Sessions of a Novel Low-Level Light Therapy Device for Home Treatment of Dry Eye Disease. Ophthalmol Ther. 2023;12(1):459-68.
10. Giannaccare G, Pellegrini M, Carnovale Scalzo G, Borselli M, Ceravolo D, Scorcia V. Low-Level Light Therapy Versus Intense Pulsed Light for the Treatment of Meibomian Gland Dysfunction: Preliminary Results From a Prospective Randomized Comparative Study. Cornea. 2023;42(2):141-4.
11. D'Souza S, Padmanabhan Nair A, Iyappan G, Dickman MM, Thakur P, Mullick R, et al. Clinical and Molecular Outcomes After Combined Intense Pulsed Light Therapy With Low-Level Light Therapy in Recalcitrant Evaporative Dry Eye Disease With Meibomian Gland Dysfunction. Cornea. 2022;41(9):1080-7.
12. Chan KE, Lau BSR, Lim BXH, Du R, Giannaccare G, Tong L, et al. Low-level light therapy and intense pulse light therapy in meibomian gland dysfunction. A systematic review and meta-analysis. Cont Lens Anterior Eye. 2024:102344.
13. Ballesteros-Sánchez A, Gargallo-Martínez B, Sánchez-González MC, Sánchez-González JM. Intense Pulse Light Combined With Low-Level Light Therapy in Dry Eye Disease: A Systematic Review. Eye Contact Lens. 2023;49(1):8-13.


Jordan Cooper (left) and Catherine Jennings are former optometry graduates and current PhD candidates with the Ocular Surface Laboratory (OSL) at the University of Auckland, working under the supervision of Professor Jennifer Craig.