The brain’s electric windows
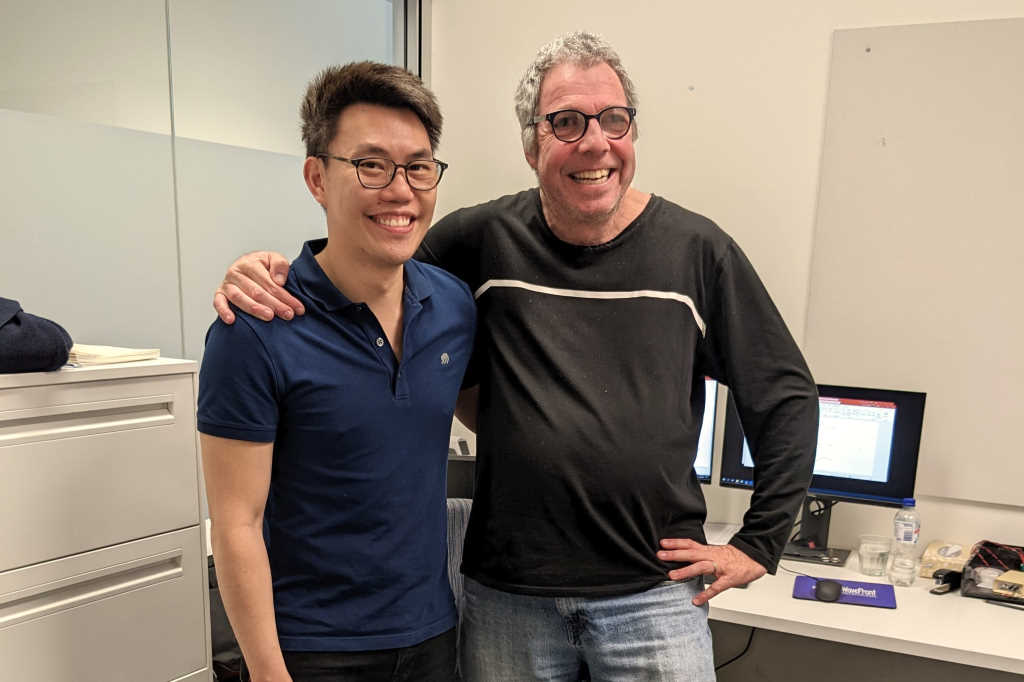
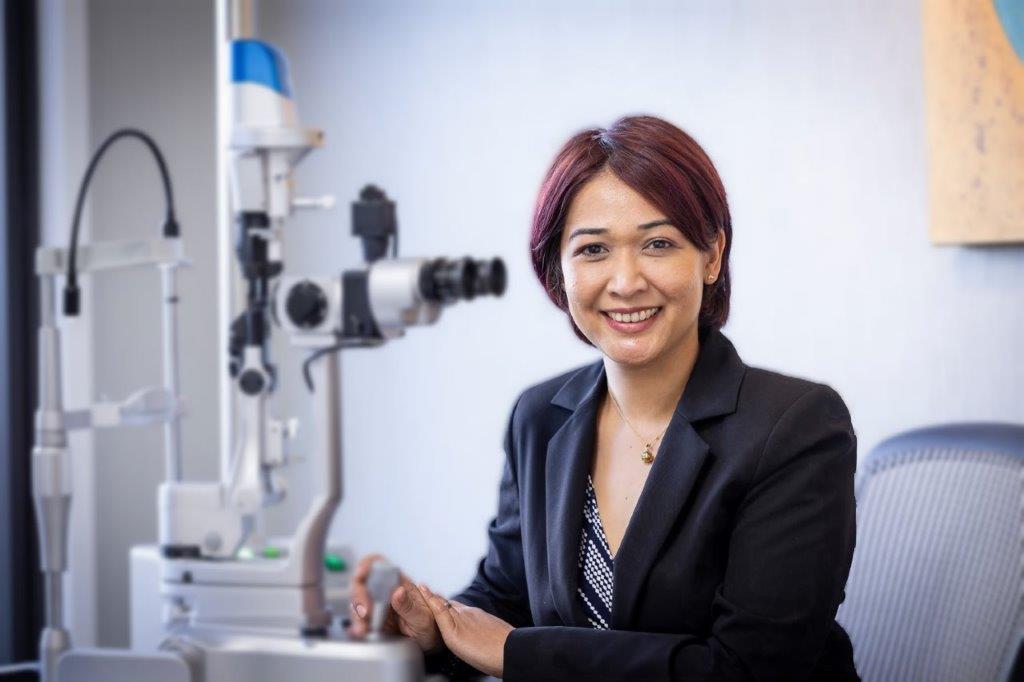
Retinal electrophysiology’s potential role in the early detection of neurodevelopmental conditions such as bipolar disorder, Alzheimer’s and autism was the subject of a recent Frontiers in Neuroscience review. Drew Jones asked the authors, University of Western Australia senior optometry lecturer Dr Jeremiah Lim and Flinders University visual electrophysiologist Dr Paul Constable, to tell him more.
How does retinal electrophysiology work and how can it be used to flag neurodegenerative disorders?
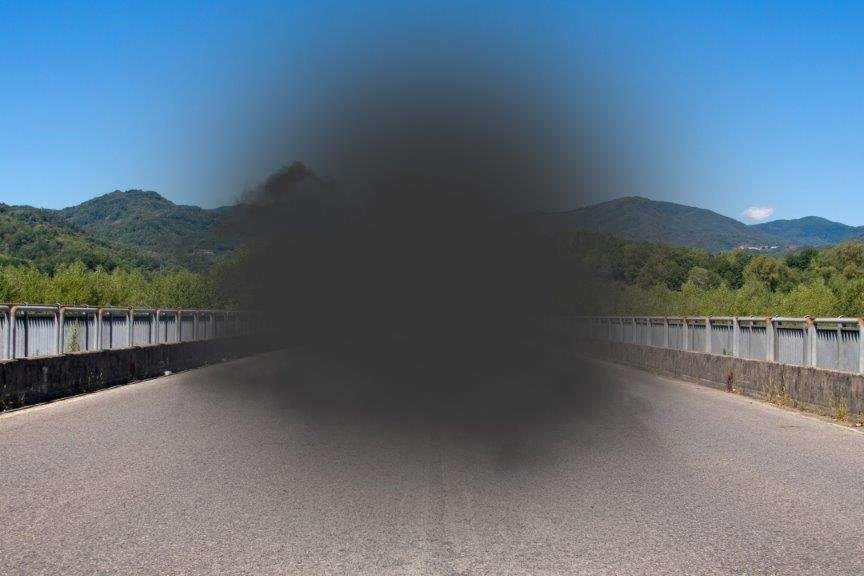
Dr Jeremiah Lim: The retina may be considered an extension of the brain as it shares the same embryogenic origins and consists of neurons and glial cells and vessels that exhibit autoregulation. We are lucky the retina is organised in layers, which was an evolutionary necessity to ensure efficiency in nutrient supply, as well as for sending information to the brain. When stimulated with light, the various cells within the lamellar structure contribute to the formation of an electrical signal known as the electroretinogram (ERG). Understanding how each component of the ERG is affected by disease allows us to generate an electrophysiological signature or biomarker. Different diseases exhibit deficits in certain areas – autism spectrum disorder (ASD) seems to affect a subset of the bipolar cells of the retina; in Parkinson’s disease, inner retinal cells such as the ganglion and amacrine cells are more affected. Our review tried to determine if there were any trends or specific biomarkers which can contribute to a diagnosis of the diseases studied.
Of the disorders discussed in your review, which are most likely to support ERG as a diagnostic tool?
JL: It’s early days, so it’s hard to say which will show the most promise. One of the findings was that certain conditions (Alzheimer’s, schizophrenia and bipolar disorder) showed better concordance in terms of ERG changes between humans and mice. This gives us some confidence that the changes observed are partially explained by an aspect of the disease mechanism seen in mouse models.
How does ERG compare with image-based screening tools for detecting conditions such as Parkinson's?
JL: Fundamentally, ERG and imaging are two sides of the same coin. ERG can be thought of as physiology or functional changes, whereas imaging, such as fundus photos and OCT, tells us more about anatomy or structural changes. Both go hand-in-hand. There are instances of eye diseases where structural changes are often detected before functional changes are seen (eg. pre-perimetric glaucoma) but often this is because of poor sensitivity of the functional test used. Since many functional and structural signs in neurological disease overlap with existing eye disease, we believe a combination of structural and functional eye signs when measured together are more likely to give rise to a unique biological signature of any given brain condition.
Could AI be used to screen ERG data in the same way it’s been applied to fundus images in diabetic retinopathy screening?
JL: Yes, there have been significant steps taken by labs in this regard, but it is not yet mainstream. My guess is eventually it will be made available by the companies selling the equipment.
Dr Paul Constable: My 2022 paper, in collaboration with UK and US researchers, described how we used machine learning and ERG to classify autism spectrum disorder (ASD). The classification accuracy of our best machine learning model using time-domain and spectral features was 86%, with 98% sensitivity, indicating spectral analysis of ERG provides helpful information for the ASD classification.
Are confounders such as smoking, diabetes, other clinical conditions and past drug use likely to be obstacles in ERG being widely adopted to identify CNS disorders?
JL: As ERG is a very sensitive tool and prone to systemic changes, many studies exclude participants with confounding factors to isolate a ‘pure’ signal which can only be explained by the presence of one disease. We know that in real life, however, this is an unrealistic expectation as people often have systemic co-morbidities as well as eye diseases that can impact the ERG waveform. Other obstacles include lack of access, either because it’s hard to find someone who does ERG or simply cost.
So could you foresee ophthalmologists and optometrists routinely performing ERGs?
JL: Currently no, as ERG equipment costs upwards of NZ$100k, not to mention electrical shielding, dark adaptation and building modifications, if you want to do it properly. It is also not very well taught at universities as most optometry schools do not have access to facilities. Outside of research, most ERGs are performed by technicians who are trained specifically for ERG, hence it is often performed in hospitals and busy eye clinics where there are enough critical patients to warrant an ERG technician. Having said that, the more recent introduction of the handheld ERG system by LKC Technologies has brought down some of the barriers in terms of cost and portability. ERGs are difficult to interpret, but the International Society for Clinical Electrophysiology of Vision can help greatly in that regard.
Do you have any ongoing ERG research?
PC: We are looking at neurodevelopmental disorders, such as ASD and ADHD, in the hope that ERG analysis can lead to better management and possibly earlier diagnoses of these conditions. We hope this may expand the clinical utility of the ERG in the not-too-distant future.