The Royal Society dry eye study
In recent years there has been growing interest in the potential link between a number of modifiable lifestyle risk factors and the development of dry eye disease, the goal being to inform cost-effective disease prevention strategies at the population level. This is important, since the public health and financial burden of dry eye disease, which is already high, is projected to rise due to ageing populations worldwide1. However, dry eye disease is also increasingly recognised to be a highly diverse and heterogenous condition2 and the risk factor profile may differ between the etiological subtypes of aqueous tear deficiency and evaporative disease. To date, there has been limited scientific literature investigating the impact of modifiable lifestyle risk factors on these disease subtypes1.
The Royal Society Summer Science Exhibition (RSSSE) is a prestigious cutting-edge research dissemination event held over the course of a week in London each year. Professor James Wolffsohn, Aston University, UK, in collaboration with members from the Ocular Surface Laboratory at the University of Auckland, won a hotly contested place at the exhibition. As well as presenting their latest research, they took the opportunity to conduct a study to explore some of the recognised gaps in the current literature on dry eye disease epidemiology, including demographic and lifestyle risk factors of aqueous deficient and evaporative dry eye disease3.
Is there a dry eye in the house?
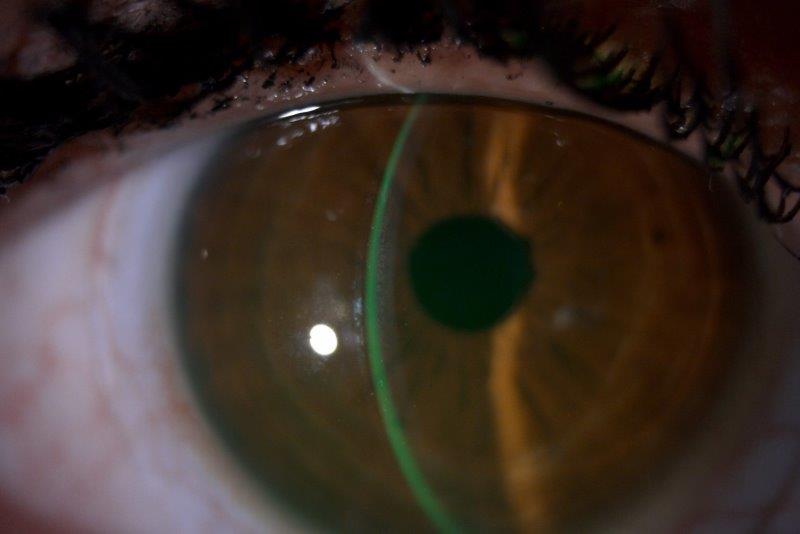
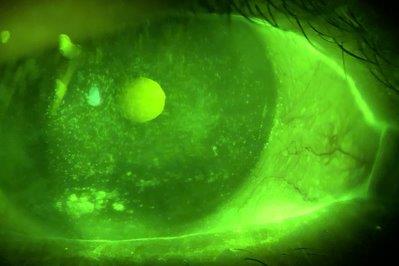
The Dry Eye exhibit at RSSSE was manned by Aston University staff and students, plus Professor Jennifer Craig, during her research and study leave pre-Covid-19. Visitors to the exhibit were recruited to complete questionnaires on lifestyle factors and dry eye symptomology, as well as assessment of ocular surface and tear film parameters using the Oculus Keratograph 5M. The diagnosis and subtype classification of dry eye disease was then determined according to the rapid non-invasive dry eye assessment algorithm, which has previously been demonstrated to exhibit high levels of diagnostic agreement with the global consensus TFOS DEWS II criteria4.
Overall, the study recruited a total of 1,125 visitors, ranging in age from five to 90 years. Dry eye disease was detected in 38% of participants, with aqueous deficient dry eye disease present in 14%, and evaporative dry eye disease diagnosed in 30%. Multivariate regression analysis was then conducted to identify independent risk factors of the two dry eye disease subtypes.
Less shut-eye = more dry eye
The results of the study showed that age, female sex, reduced sleep duration, higher psychological stress and decreased self-perceived health status were independently associated with aqueous deficient dry eye disease. These findings are consistent with earlier studies that have demonstrated an association between dry eye disease and sleep disorders, decreased sleep duration and quality5. The underlying mechanisms behind the association are not fully understood, but might involve a number of neurohormonal factors, including decreased parasympathetic tone, as well as a change in the hypothalamic-pituitary-adrenal axis and renin-angiotensin-aldosterone system5.
The study also identified a number of risk factors for the evaporative form of dry eye disease, including advancing age, East and South Asian ethnicity, contact lens wear, increased digital device screen exposure, increased psychological stress and poorer self-perceived health status. These trends were in agreement with those reported in existing literature, including the well-established association between contact lens wear and dry eye disease, which is thought to be mediated largely by the disruption of the surface tear film lipid layer that leads to accelerated rates of aqueous tear evaporation6. The link between increased digital screen exposure and the development of dry eye disease is thought to be related to suppression of the blink reflex and consequent reduction in blink rate and quality during prolonged visual concentration7.
References
- Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15(3):334-365.
- Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276-283.
- Wolffsohn JS, Wang MTM, Vidal-Rohr M, et al. Demographic and lifestyle risk factors of dry eye disease subtypes: A cross-sectional study. Ocul Surf. 2021;21:58-63.
- Wang MTM, Xue AL, Craig JP. Screening utility of a rapid non-invasive dry eye assessment algorithm. Cont Lens Anterior Eye. 2019;42(5):497-501.
- Au NH, Mather R, To A, Malvankar-Mehta MS. Sleep outcomes associated with dry eye disease: a systematic review and meta-analysis. Can J Ophthalmol. 2019;54(2):180-9.
- Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511-538.
- Wang MTM, Chan E, Ea L, et al. Randomized Trial of Desktop Humidifier for Dry Eye Relief in Computer Users. Optom Vis Sci. 2017;94(11):1052-1057.


Professor James Wolffsohn (right) is part of the Optometry & Vision Science Research Group (OVSRG), Aston University, UK. Dr Michael Wang (left) is a neuro-ophthalmology clinical research fellow in the Department of Ophthalmology at the University of Auckland.