The truth in black and white
An 88-year-old man’s referral letter stated the following diagnosis:
- Bilateral pseudophake with vitrectomy peel each eye and previous left macular hole secondary to vitreomacular traction
- Longstanding bilateral wet age-related macular degeneration (AMD), on treatment with Avastin, plus multiple areas of dry atrophy
- Oblique prism required for double vision
- Stroke causing right homonymous superotemporal quadrantanopia six months earlier
- Visual acuity (RE) 6/15, (LE) 6/12
- Cannot read with current glasses. Has tried a simple magnifier but does not find it satisfactory.
A preliminary phone call to this patient sent my head spinning as he kept insisting that his vision had been “fine” until he had the stroke. Since then, he was not sure if he was allowed to drive and could not read because his new glasses were no better than his old ones, which he had continued to wear. He said the optometrist had kept taking his new ones back to change the lenses, but kept getting them wrong because he still couldn’t read his newspaper with either pair.
Alarm bells started ringing in my head and I suddenly remembered why I left my optometry practice. I contacted his optometrist and delicately requested both new and previous prescriptions, for comparison.
Latest prescription:
(R) +1.50 –3.50 x 95, 6.5 dioptres prism, base out; 1.75 dioptre prism, base down R
(L) +0.75 –3.25 x 90, 6.0 dioptres prism, base out; 1.75 dioptres, base up L
Add +3.25 right and left for near.
Previous prescription:
(R) +1.50 –2.50 x 92, 4.5 dioptres, base out; 1.5 dioptres, base down
(L) +0.50 –2.50 x 90, 4.5 dioptres, base out; 1.5 dioptres, base up
Add +2.50 right and left.
Comparing the two prescriptions, both in bifocal form, gave me some insight as to what may have happened since his stroke. Not only did he now have a right homonymous quadrantanopia, but his longstanding binocular problems had greatly worsened as his brain tried to regain control of his binocular co-ordination.
His driving issue was obvious, so I decided to leave the quadrantanopia and possible diplopia to his ophthalmologist, while I tackled the reading problem. Since he had longstanding AMD treated with six-weekly Avastin injections, which had reduced his distance acuity to marginally within the driving limit, the AMD was clearly the primary cause of his reading difficulty. I could assume that the stroke may have caused some additional loss of contrast sensitivity function, which would exacerbate the problem.
Returning to the comparison of the before and after prescriptions, I noted the reading add had been increased from +2.50 to +3.25, presumably to give him more magnification and allow for the increased cyl, but that would come at a closer working distance.
This man was having trouble aligning his eyes to minimise diplopia when he looked into the distance, let alone when attempting to converge them to line up for reading at close range. Maybe this was adding to the problem he’d had with his reading? Certainly it was adding to the optometrist’s problem with multiple lens remakes to attempt to get this man comfortable in his visual function, as well as his mental state!
I anticipated this was going to be a long and difficult consultation. I was not wrong!
Assessment findings
Binocular functional visual field showed an absolute superior right quadrantanopia extending to 5° from the point of fixation, with an additional relative scotoma (fading of the target) extending to within 2.5° from the central point. No surprises there, though fading in close to the fixation point would cause some blur, patchiness or loss of letters at the end of words and lines of print, leading to some confusion, particularly if his binocular single vision is not being maintained.
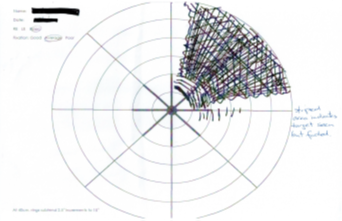
Visual field scan of the 88-year-old man
As I went to measure his reading ability, I observed him closing his right eye to read and he commented that this had been concerning him. “Why am I not surprised?” I thought to myself, but bottled it as I needed to get him to concentrate on reading.
His binocular near acuity was N 20 on a high-contrast single word chart in average room lighting. This improved to N 6 with intense local lighting but declined a little to N 10 with a continuous-text reading card. This was unusual, as the continuous-text acuity is usually a little better than single-word acuity. Perhaps the extra cognitive load was too much for him?
His low-contrast acuity on the same continuous-text card was greatly reduced to being unable to read N 80. As anticipated, the stroke had taken a toll here and is why his acuity improved so markedly when I applied local light.
Based on these measurements, I assessed this gentleman as needing approximately 2–3 times magnification, together with maximal light or other contrast enhancement to assist him to read his newspaper.
Let battle commence
Finding the right solution for him required a lot of patience and coaxing to get him to accept that all magnifiers have to be moved in some manner and there is a finite limit to how big the lens of a magnifier can be manufactured.
His main issue initially was coming to terms with the idea that his new prescription glasses were not going to solve the visual problems that were due to his AMD and co-ordination problems. This was exacerbated by the stroke, which appears to have caused further loss of contrast sensitivity, as well as upsetting the binocular co-ordination, in addition to the quadrantanopia, which he now appears to be getting used to. Since his corrected acuity is quite similar between right and left eye, there is interference between right and left, which is difficult to suppress.
In a bifocal lens the prism remains the same for distance viewing or near – it cannot be altered separately. We discussed the possibility of getting a pair of single-vision reading glasses with the prism adjusted to get single vision at the required reading distance. I doubt it will make any difference in terms of clarity, but he may be more comfortable that way (although it would be a very chunky pair of lenses). On the other hand, he has worn bifocals for a long time and may find single-vision glasses difficult to get used to, particularly the inconvenience of changing glasses whenever he has to look farther away.
He finally conceded that a 2.8-times LED illuminated stand magnifier was helpful to enable him to read his newspaper from cover to cover and do the crossword. I adroitly (I think) side-stepped any discussion on whether he should revisit his optometrist to return his new glasses.

Naomi Meltzer is an optometrist who runs an independent practice specialising in low-vision consultancy. She is a regular contributor to NZ Optics.