Toxoplasmosis: what is new in 2023?
Toxoplasma retinochoroiditis is a vision-threatening disease and a major cause of posterior uveitis worldwide. It is a protozoan parasite infection of Toxoplasma gondii, which typically affects one eye of a young individual, with a mean age of 29.5 years at first presentation1. Although it can infect any part of the retina, over half of all involvement is in the posterior pole1.
Diagnosis
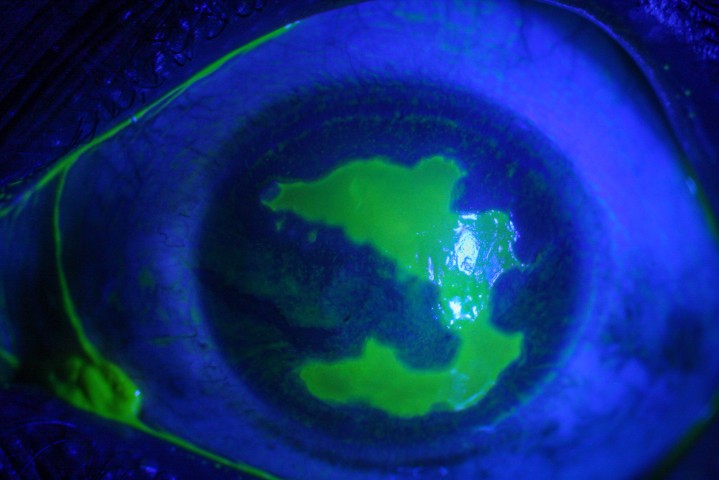
Classically, toxoplasmosis presents as an area of active retinitis adjacent to a chorioretinal scar (Fig 1, see main picture). In such cases a diagnosis can be made clinically.
Atypical features include multifocal retinitis, bilateral involvement, papillitis, juxtapapillary exudative lesions, infection limited to the outer retina and severe vitritis. In such cases a clinical diagnosis is difficult to make. Atypical cases are more likely in immunosuppressed individuals. As with atypical presentations, focal retinitis without adjacent chorioretinal scar, occurring in 28% of cases2, can also pose diagnostic uncertainty (Fig 2).
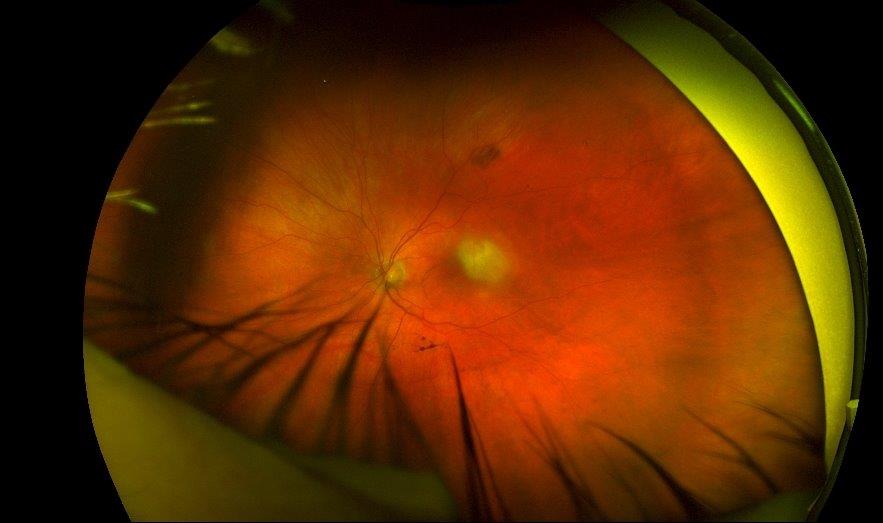
Fig 2. Toxoplasma retinochoroiditis without adjacent scar
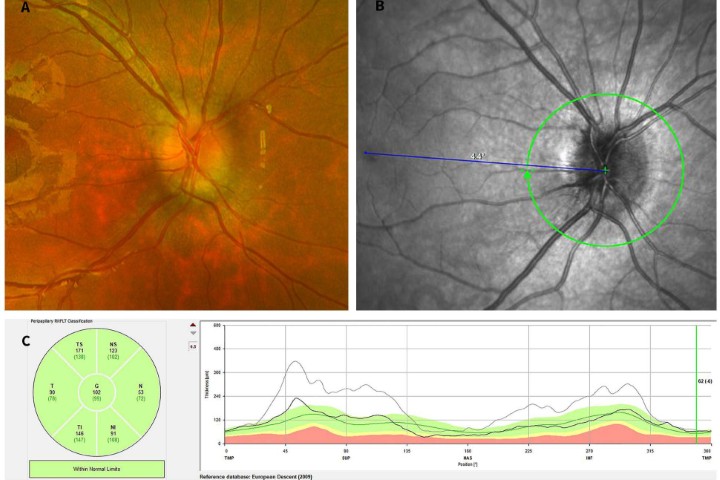
Multimodal imaging and laboratory investigations can assist in diagnosis, especially in atypical cases. In particular, optical coherence tomography (OCT) can assist in early diagnosis while waiting for laboratory results. OCT morphologic features have been validated in various case series (Table 1; Fig 3 & 4)3.
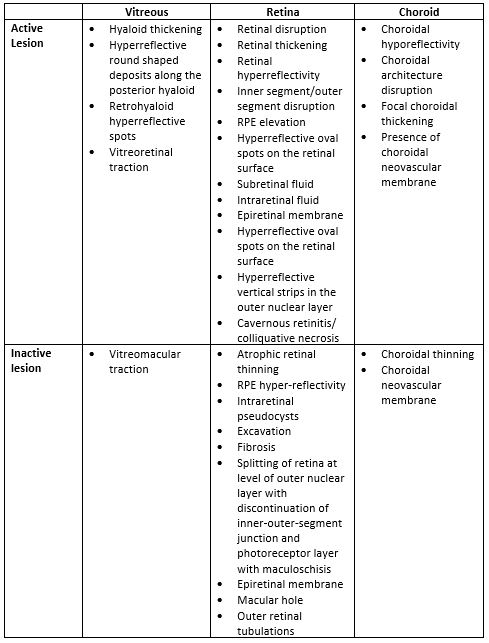
Table 1. Typical OCT Findings in toxoplasma retinochroiditis
Serologic testing has a limited role in the diagnosis of toxoplasma retinochoroiditis due to the high prevalence of seropositivity. Additionally, immunoglobulin M (IgM) is detectable 7-14 days after acute infection and if tested too early it can yield a false negative result.
Ocular fluid PCR is a valid technique, particularly for atypical presentation, with a specificity of 89%4. The sensitivity varies in the literature, possibly related to inter-laboratory differences in testing methods (conventional PCR, real-time PCR, multiplex PCR, nested PCR), subject immune status and site of sampling.
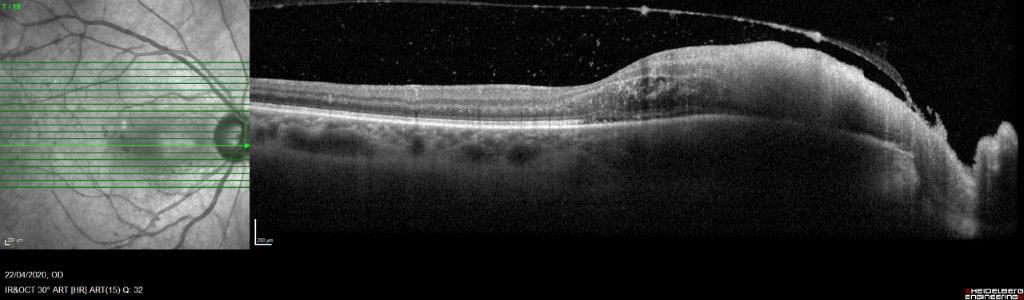
Fig 3. OCT imaging of active toxoplasma retinochoroiditis showing disruption of retinal layers, retinal thickening, retinal hyperreflectivity, RPE elevation, focal choroidal thickening, choroidal hyporeflectivity, hyaloid thickening, hyperreflective round shaped deposits along the posterior hyaloid, retrohyaloid hyperreflective spots, cavernous retinitis
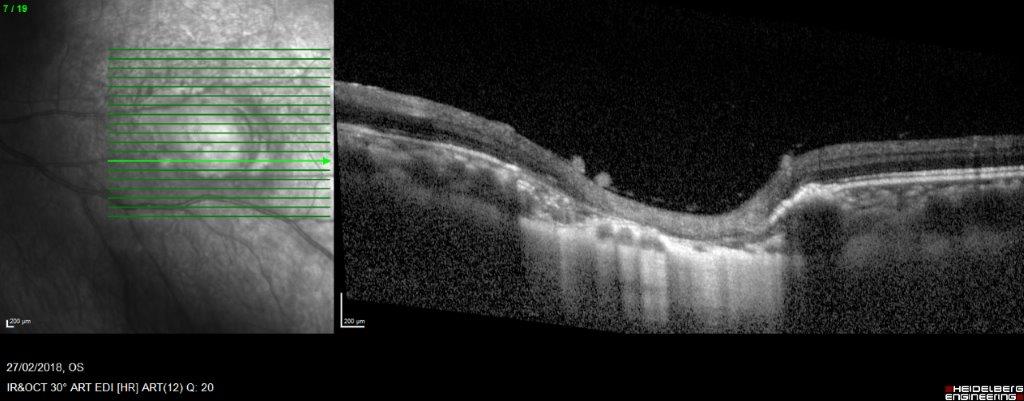
Fig 4. OCT through inactive lesion showing atrophic retinal thinning, RPE hyperreflectivity, retinal excavation and choroidal thinning
A vitreous tap is suggested to be the most suitable site of sampling for PCR testing due to its contact with the retinochoroidal infective focus4. However, since most subjects are young with dense vitreous, it may be difficult to aspirate and risks inducing retinal tears. Aqueous tap may be safer and more reliable. The sensitivity of toxoplasma retinochoroiditis detection in vitreous has been reported at 97.5% and 81.5% in aqueous5.
Treatment
Treatment is individualised with the aim of treating the underlying disease, inflammation and any complications. In immunocompetent subjects, toxoplasma retinochoroiditis is a self-limiting disease, healing with residual chorioretinal scar within 6-8 weeks. Thus, some clinicians treat only selected manifestations, while others advocate treating all cases in an attempt to reduce complications. The natural course of the infection, secondary complications, immune status and possibility of drug toxicity to antiparasitic drugs all need to be considered and weighted.
Vision-threatening factors warranting treatment include:
- Immunocompromised patient status
- Significant reduction in visual acuity
- Location of active lesion at macular, disc, adjacent to large blood vessels
- Significant vitreous haze
- Presence of macular oedema
- Presence of optic disc oedema
- Presence of vascular occlusion
- Atypical presentations
Treatment includes antibiotics and corticosteroids and is usually maintained for 4-6 weeks. Antibiotics destroy the bradyzoites but not the cysts, therefore the goal of antimicrobial treatment is to stop parasitic multiplication during active retinitis to limit the size of the eventual chorioretinal scar. Various antibiotics have been used, with parameters including patient allergies, pregnancy, immune status and possible drug adverse effects influencing the choice (Table 2). Co-trimoxazole tends to be favoured as it is readily available and well tolerated.
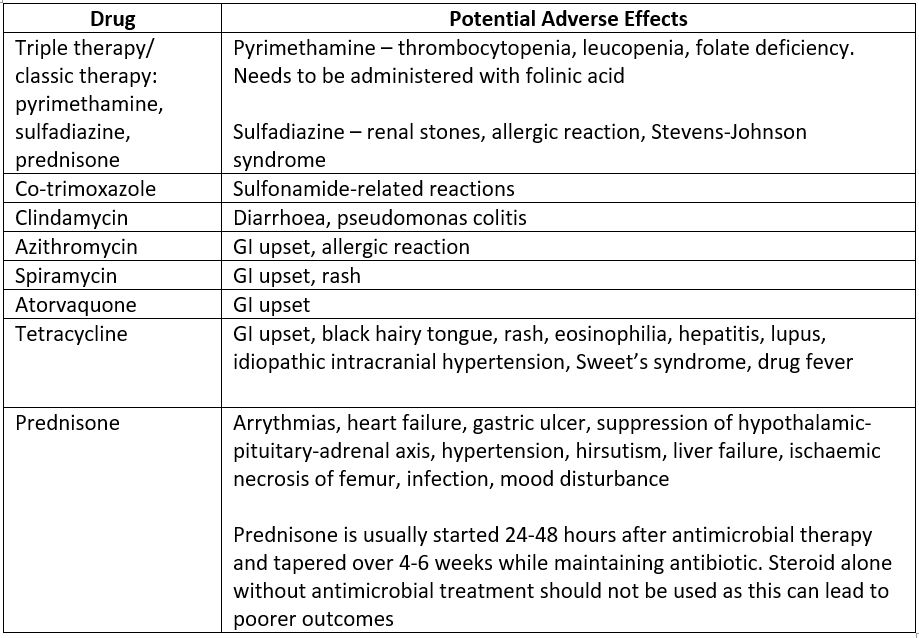
Table 2. Antibiotic options for toxoplasma retinochoroiditis
Intravitreal treatment, comprising of clindamycin 1mg with or without dexamethasone 0.4mg, has been shown to be as effective as triple therapy6 and can be considered as an adjunct for fovea involving infective foci.
The role of prophylaxis
Recurrence may be observed in up to 25% of cases in the first two years7. This is due to the release of tachyzoites from resident cysts2. With every recurrence, the probability of visual impairment increases.
Co-trimoxazole 960mg every three days was shown to reduce the recurrence rates from 23.8% to 6.6% over 20 months in non-HIV patients with two or more episodes of toxoplasma retinochoroiditis8. Co-trimoxazole should be considered in a subject with multiple recurrences, those with persistent immunosuppression and in macular-involving toxoplasmosis. The ideal duration of prophylactic treatment has yet to be defined, although prophylactic treatment for 311 days after initial infection has been shown to significantly reduce the risk of recurrence over a six-year follow-up9.
Infection in pregnancy
Toxoplasma infection in pregnancy requires multidisciplinary input from ophthalmologists, obstetricians and infectious disease specialists.
Management depends on whether the infection is a reactivation or a primary acquired infection, and thus requires serologic investigation of the pregnant woman. Reactivation of latent infection acquired before gestation does not present a risk to the developing foetus, while toxoplasmosis that is initially acquired during pregnancy can have devastating teratogenic consequences.
Reactivation
Certain systemic antimicrobial agents are potentially teratogenic. The highest risk of adverse effects from antimicrobial drugs is associated with the first trimester. Thus, the ideal treatment in pregnancy is as little antimicrobial as possible with a strong consideration for not treating unless there is vision-threatening disease. The next best option is local therapy with intravitreal clindamycin with or without intravitreal dexamethasone.
Spiramycin is also a systemic medication that is safe to use during pregnancy. Alternative options include azithromycin and clindamycin. It is important to consult the latest safety information before prescribing medication in pregnancy and breastfeeding.
Primary acquired infection
The risk of congenital infection and severity depends on the gestational age at which the infection is acquired. There is an inverse relationship between transplacental transmission and the severity of congenital disease. The earlier the infection occurs in pregnancy, the lower the risk of congenital infection, but the greater the severity of congenital disease. In primary acquired infection, treatment is required not only for the ophthalmic disease but also to reduce the risk of transmission to the foetus.
Amniotic fluid PCR is effective for prenatal diagnosis of congenital toxoplasmosis with a specificity and positive predictive value of 100% and sensitivity of 70-95%, depending on gestational age4.
Classic therapy is contraindicated as pyrimethamine is teratogenic and sulfadiazine can cause bilirubin encephalopathy. Spiramycin reduces the risk of vertical transmission and is used throughout pregnancy.
Toxoplasmosis mind control!
One of the most fascinating aspects of various parasites is their ability to manipulate aspects of the host’s behaviour in an attempt to gain parasitic survival advantage. Toxoplasma has been suggested to be one such parasite.
In humans, toxoplasmosis has been linked to neuropsychiatric disorders, including schizophrenia and depression; neurocognitive disorders, including personality disorders; and poorer neurocognitive performance, including slower reaction times and poor concentration10,11. Poor impulse control, including violent risk-taking behaviours, non-suicidal self-injury and attempted suicide have been associated with toxoplasmosis11.
Proposed mechanisms of mind control include alterations in neurotransmitters, particularly increased dopamine levels, changes in hormones such as elevated testosterone levels, and altered metabolites and immune responses, including expression of cytokines and IL-1alpha11.
Evidence of definitive parasitic mind control is, however, still inconclusive. Observations of neuropsychiatric and neurocognitive change with Toxoplasma infection may merely be an association rather than a causative effect. Experimental studies using animal models provide the most convincing evidence of the parasite’s ability to hijack the host’s mind.
Infected rodents spend more time in open pen areas and demonstrate an attraction to feline odour; these behaviours increase predation risk12,13,14,15 and chances of the host being consumed by the feline, thus allowing Toxoplasma gondii to complete its lifecycle. This behaviour modification in modern humans is suggested to be a side effect of infection or a residual effect from a time when human ancestors were still under predatory threat from felines16.
Conclusion
Toxoplasma retinochoroiditis is common. While serology has limited utility it can be helpful – if IgM is positive, it shows recent infection; if negative, it can be ruled out. Intraocular PCR is an important diagnostic tool in clinical practice, particularly in atypical presentations. OCT imaging is convenient, readily available and allows early diagnosis at the time of presentation and thus early initiation of appropriate antimicrobial therapy. Intravitreal clindamycin is a useful adjunct for macular lesions and for pregnant and breastfeeding individuals. Prophylactic co-trimoxazole should be considered, particularly for macular lesions given the high recurrence rates.
References
- Butler NJ, Furtado JM, Winthrop KL, et al. Ocular toxoplasmosis II: clinical features, pathology and management. Clin Exp Ophthalmol. 2013; 41(1):95-108
- Bosch-Driessen LEH, Berendschot TTJM, Ongkosuwito JV, et al. Ocular toxoplasmosis: clinical features and prognosis. Ophthalmology. 2002; 109(5): 869-878
- Invernizzi A, Agarwal AK, Vittoria R, et al. Comparing optical coherence tomography findings in different aetiologies of infectious necrotising retinitis. Br J Ophthalmol. 2018; 102(4):433-7.
- Kalogeropoulos D, Sakkas H, Mohammed B, et al. Ocular toxoplasmosis: a review of the current diagnostic and therapeutic approaches. Int Ophthalmol. 2022; 42(1):295-321.
- Farhadi A, Haniloo A, Fazaeli A, et al. PCR-based Diagnosis of Toxoplasma Parasite in Ocular Infections Having Clinical Indications of Toxoplasmosis. Iran J Parasitol. 2017;12(1):56-62.
- Soheilian M, Ramezani A, Azimzadeh A, et al. Randomized trial of intravitreal clindamycin and dexamethasone versus pyrimethamine, sulfadiazine, and prednisolone in treatment of ocular toxoplasmosis. Ophthalmology. 2011;118(1):134-41
- Wadhwa H, Sims JL, Niederer RL. Rate of recurrence of toxoplasmosis retinochoroiditis at a tertiary eye centre in Auckland. NZ Med J. 2022; 135(1553)
- Silveira C, Belfort R Jr, Muccioli C, et al. The effect of long-term intermittent trimethoprim/sulfamethoxazole treatment on recurrences of toxoplasmic retinochoroiditis. Am J Ophthalmol. 2002;134(1):41-6.
- Fernandes Felix J, Cavalcanti Lira R, Grupenmacher A, et al. Long-term Results of Trimethoprim-Sulfamethoxazole Versus Placebo to Reduce the Risk of Recurrent Toxoplasma gondii Retinochoroiditis. Am J Ophthalmol. 2020; 213:195-202
- Sugden K, Moffitt T, Pinto L, et al. Is Toxoplasma Gondii Infection Related to Brain and Behavior Impairments in Humans? Evidence from a Population-Representative Birth Cohort. PLoS One. 2016;11(2):e0148435
- Johnson S, Johnson P. Toxoplasmosis: Recent Advances in Understanding the Link Between Infection and Host Behavior. Annu Rev Anim Biosci. 2021;9:249-264.
- Gatkowska J,Wieczorek M, Dziadek B, et al. Behavioral changes in mice caused by Toxoplasma gondii invasion of brain. Parasitol Res. 2012; 111(1):53–58
- Berdoy M, Webster J, Macdonald D. 2000. Fatal attraction in rats infected with Toxoplasma gondii. Proc Biol Sci. 2000; 267(1452):1591–94
- Vyas A, Kim S-K, Giacomini N, et al. Behavioral changes induced by Toxoplasma infection of rodents are highly specific to aversion of cat odors. Proc Natl Acad Sci USA. 2007;104(15):6442–47
- Bezerra E, dos Santos S, Coelho dos Santos T, et al. Behavioral evaluation of BALB/c (Mus musculus) mice infected with genetically distinct strains of Toxoplasma gondii. Microb Pathog. 2019;126:279–86

Dr Priya Samalia is currently an ophthalmologist with subspecialty training in medical retina and uveitis, based in Christchurch.

Dr Rachael Niederer currently works as a senior lecturer at the University of Auckland and as an ophthalmologist at Te Whatu Ora Auckland and Auckland Eye, specialising in uveitis and medical retina.