Unravelling glaucoma using modern genetics
Artificial intelligence (AI) is now a part of our daily lives – it's not just about predicting which movie you'll binge next, finding the fastest route home, or powering tools like ChatGPT. In our AI-driven world, where machine learning and algorithms have become familiar conveniences, there is a lesser-known revolution unfolding. The same cutting-edge technology that personalises our digital experiences is now transforming our understanding of health and disease.
One such frontier is the fusion of AI, bioinformatics and genetics – a fascinating field that is reshaping how we approach diseases like glaucoma, a leading cause of blindness worldwide. Our genes hold intricate secrets about our health, and these secrets are being unlocked with remarkable precision. While companies like 23andMe have brought genetic testing into our homes, offering insights into ancestry and health risks, this is just the beginning of what advanced genetic research can reveal.
Small changes, big impact
When we discuss genetics, we often talk about changes to a gene or set of genes as the primary players, like the headlines claiming “Glaucoma-associated myocilin: a better understanding but much more to learn”1. And while this is true – mutations in the myocilin gene (MYOC) can have a dramatic effect on overall glaucoma risk – it is often the small variations within and surrounding these genes that can make a big (or small) difference in our health. These tiny differences, known as single nucleotide polymorphisms (SNPs, pronounced ‘snips’), are single base-pair changes in the DNA sequence, affecting how genes function and thus contributing to disease susceptibility.
Imagine your DNA as a long string of letters, each representing a genetic instruction. Your genome has about three billion of these letters. SNPs are the specific points within them where small changes (like typos) have evolved over time across different populations2. Most of the time they’re harmless, but sometimes they can subtly alter the way your body functions, with a small subset collectively leading to health disparities. When it comes to diseases such as glaucoma, certain SNPs can increase your risk, even if the changes seem minor.
Reading the clues
Polygenic risk scores (PRS) are a way of reading the clues left by these SNPs. Rather than looking at just one or two genetic changes, a PRS considers thousands of SNPs scattered throughout your DNA. Each individual SNP might add only a tiny amount to your overall risk of developing a disease like glaucoma – some protecting you, some harming you. But when you add up those thousands of small effects, they quickly add up to meaningful changes, providing a clearer picture of your genetic predisposition3. Decades of work have shown that an individual’s genetics don’t equate to destiny, but they can be enough to push you in a certain direction.
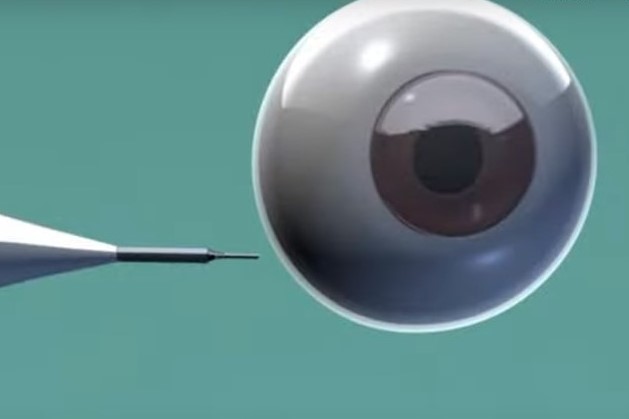
This is particularly important for a condition like glaucoma – a term referring to a group of eye conditions characterised by damage to the optic nerve and leading to vision loss. Globally, glaucoma is one of the leading causes of permanent blindness, with the most prevalent subtype, primary open-angle glaucoma (POAG), affecting 70 million individuals worldwide4. Often referred to as ‘the silent thief of sight’, glaucoma can progress without any noticeable symptoms (see Fig 1). It is estimated up to half the number of people with glaucoma won’t know it until after meaningful changes to their vision. There is no current gold-standard cure.

Fig 1. Diagram of glaucoma subtypes. Anatomical and physiological differences between a normal eye (a), and eyes exhibiting either POAG (b) or PACG (c). This illustration highlights the flow of aqueous humour (yellow arrows) and anatomical distinctions that differentiate between the glaucoma subtypes
By analysing SNPs through PRS, we can identify people at higher risk long before any symptoms appear, which offers a more refined risk assessment and a chance for early screening and intervention (glaucoma has many useful management strategies). Conversely, PRS is also beginning to alleviate concerns for individuals identified as having below-average genetic risk. For these patients, knowing their decreased or lower-than-population-average risk can reduce anxiety and help them focus on general health and lifestyle modifications rather than intensive glaucoma screening or treatments.
PRS in a large population cohort – a case study
The ability to decode these tiny genetic variations has evolved dramatically in recent years. Advances in bioinformatics and genetic research have given us tools that were once science fiction. Today, vast databases exist around the world where the genetic information of hundreds of thousands (or millions) of individuals can be combed through, providing hints for researchers as to the origins of disease risk. AI and sophisticated algorithms play a pivotal role in this, processing vast amounts of genetic data with incredible speed and accuracy, allowing us to generate detailed risk profiles5.
Our research focused on the development and validation of PRS models using data from the UK Biobank cohort, which included 13,247 glaucoma cases and 373,537 controls. We started with data from the latest genome-wide association studies (GWAS) for POAG to identify SNPs associated with the disease (see Fig 2). Then, employing the latest software tools PRSice-2 and PLINK, we calculated a PRS as a weighted sum of these risk alleles using effect sizes from GWAS results. To ensure the robustness of the PRS and reduce redundancy, we applied clumping (to exclude SNPs that were in high linkage disequilibrium with each other) and thresholding (to include only the most significant SNPs from the GWAS). In the end, our model identified over 2,500 SNPs that contributed to the final model.

Fig 2. Overview of the PRS model. A visual representation illustrating the sequential process of identifying risk loci through GWAS, developing a PRS model using data from the UK Biobank cohort, and stratifying samples based on PRS to assess genetic susceptibility to various conditions (figure constructed using Biorender)
As shown in Fig 3, the standardised normal distribution (SND) plot illustrates the distribution of PRS in individuals with glaucoma (cases) compared to those without (controls). The plot clearly demonstrates that individuals with glaucoma tend to have higher PRS than those without, highlighting the genetic risk differences between the two groups. This suggests that PRS could be a valuable tool for identifying individuals at higher genetic risk for glaucoma and may aid in early detection strategies.

Fig 3. SND curve derived from a PRS model, illustrating the distribution of scores for cases (orange) and controls (blue)
Work to build better models is still ongoing, but our current model is able to predict glaucoma outcomes with relatively high accuracy just by looking at an individual’s PRS, along with common demographic factors such as age and sex. Our model was particularly adept at identifying individuals with higher PRS who had been diagnosed at an earlier age, had a history that included medical intervention (glaucoma surgery or medication), or exhibited worse markers of disease such as elevated intraocular pressure (IOP) or thinner retinal nerve fibre layers. When we factored in these clinical markers, we observed a noticeable improvement in the model’s area under the curve (AUC), indicating its enhanced predictive power. This highlights the role of genetic risk not only as an indicator of disease onset but also as a predictor of disease severity. Therefore, individuals with higher genetic risk may not just be more likely to develop glaucoma but may also face higher likelihood of experiencing more severe or rapid progression of the disease.
These findings demonstrate how computer-driven predictions can help in assessing one’s likelihood of developing glaucoma based on their unique genetic makeup, thus facilitating proactive measures and personalised care. For instance, individuals with high genetic risk may benefit from earlier screening, frequent monitoring or adjusting treatment intensity based on their cumulative genetic risk/PRS. By incorporating PRS into our routine health assessments, we can move towards a future where preventive measures and treatments are tailored specifically to our genetic profiles, ultimately leading to earlier interventions and more effective use of healthcare resources6.
Insights from two key studies
To contextualise our current PRS model, we compared it to the PRS models developed as part of two other well-known glaucoma studies. One, developed by Professor Jamie Craig’s team in Australia in 2020, is widely regarded as the gold standard of PRS in the glaucoma research space7. By leveraging the multi-trait analysis of genome-wide association study (MTAG) method, which combines genetically correlated traits (including IOP and vertical cup-disc ratio) to improve genetic risk prediction, their team created a PRS model with significant predictive power. Their PRS model was validated in multiple cohorts, including the UK Biobank and Blue Mountains Eye Study, achieving an impressive AUC of 0.8 (80% predictive power to detect glaucoma cases versus controls).
The second well-regarded glaucoma PRS model, developed by Dr Deborah Thompson’s team used UK Biobank data to create phenome-wide PRS models across 28 different diseases (including glaucoma) and an additional 25 quantitative traits8. This approach focused on a PRS methodology that incorporated multiple phenotypes and ancestries to develop a broader set of predictive models. For each trait/phenotype, they applied a Bayesian method, which allowed for the integration of prior knowledge and probabilities to estimate more accurate risk scores based on observed data. Unlike Prof Craig’s 2020 PRS, Dr Thompson’s work prioritised population diversity and a phenome-wide approach, reporting an AUC of 0.649 for glaucoma. It is important to note that Dr Thompson’s 2022 study is currently available only as preprint, yet to undergo the peer review process.
Together, these two studies highlight the rapid advancement of PRS research and versatility of methodologies. They also illustrate the importance of validating PRS models across diverse cohorts and methods, ultimately paving the way for more robust and accurate predictions in the future of glaucoma research.
Caveats and limitations
As promising as this all sounds, it’s important to acknowledge several current caveats. Genetics is only one piece of the puzzle when it comes to disease risk. For instance, a high PRS doesn’t guarantee that someone will develop glaucoma, just as a low PRS doesn’t mean they’re completely in the clear. Environmental factors and lifestyle choices such as air pollution, smoking and diet have also been shown to have significant association with the risk of developing glaucoma9-11.
Another key challenge is the interpretation of PRS across different populations. Many of the largest cohorts used for genetic research, including those that form the basis of glaucoma PRS, are heavily weighted towards populations of European ancestry (including major studies in the US, UK and Australia). As genetic ancestry has a large role in which SNPs an individual might have inherited (what’s common in one population might not be common in another), the risk predictions are still evolving to achieve accuracy across people of all genetic ancestries. Expanding research to include trans-ethnic populations is crucial for making PRS a universal healthcare tool.
There is also the matter of how this information is used. The idea of knowing your genetic risk can be empowering, but it can also be daunting. The psychological burden of discovering that you are at high risk for a disease like glaucoma isn’t something to take lightly. For this reason, it is crucial that genetic information is paired with appropriate counselling and support, ensuring that individuals are equipped to make informed decisions about their health.
Conclusion
As we look to the future, the role of genetics and AI in healthcare is only set to grow. The ability to predict health risks through all available information (including clinical and genetic data) marks a new era in medicine. In the near future, later-in-life diseases like glaucoma will be treated through a proactive approach, rather than the current, predominantly reactive, approach. By embracing the insights offered by PRS and other genetic tools we can start to take control of our health in ways that were unimaginable just a few decades ago, mitigating changes in the retina before they ever become a problem to eyesight.
References
- Resch ZT, Fautsch MP. (2009). Glaucoma-associated myocilin: a better understanding but much more to learn. Exp Eye Res, 88(4), 704-712.
- Shen H, Li J, Zhang J, Xu C, Jiang Y, Wu Z, Zhao F, Liao L, Chen J, Lin Y, Tian Q, Papasian CJ, Deng H-W. (2013). Comprehensive characterization of human genome variation by high coverage whole-genome sequencing of forty-four Caucasians. PloS One, 8(4), e59494.
- Choi SW, Mak TSH, O’Reilly PF. (2020). Tutorial: a guide to performing polygenic risk score analyses. Nat Protoc, 15(9), 2759-2772.
- Tham YC, Li X, Wong TY, Quigley HA, Aung T, Cheng CY. (2014). Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology, 121(11), 2081-2090.
- Lewis CM, Vassos E. (2020). Polygenic risk scores: from research tools to clinical instruments. Genome Med, 12(1), 44.
- Gao XR, Huang H, Kim H. (2019). Polygenic risk score is associated with intraocular pressure and improves glaucoma prediction in the UK Biobank cohort. TVST, 8(2), 10-10.
- Craig JE, Han X, Qassim A, Hassall M, Cooke Bailey JN, Kinzy TG, MacGregor S et al. (2020). Multitrait analysis of glaucoma identifies new risk loci and enables polygenic prediction of disease susceptibility and progression. Nat Genet, 52(2), 160-166.
- Thompson DJ, Wells D, Selzam S, Peneva I, Moore R, Sharp K, Weale ME et al. (2022). UK Biobank release and systematic evaluation of optimised polygenic risk scores for 53 diseases and quantitative traits. MedRxiv, 2022-06.
- Li L, Zhu Y, Han B, Chen R, Man X, Sun X, Lei Y et al. (2022). Acute exposure to air pollutants increase the risk of acute glaucoma. BMC Public Health, 22(1), 1782.
- Li Y, Hecht SS. Carcinogenic components of tobacco and tobacco smoke: A 2022 update. Food Chem Toxicol. 2022 Jul;165:113179. Epub 2022 May 25. PMID: 35643228; PMCID: PMC9616535..
- Al Owaifeer AM, Al Taisan AA. (2018). The role of diet in glaucoma: a review of the current evidence. Ophthalmol Ther, 7, 19-31.

Sirithi Medagoda is a data scientist with a master’s degree working at the University of Auckland.

Dr William Schierding is a bioinformatician at the University of Auckland, specialising in predictive models and AI in glaucoma.

Professor Helen Danesh-Meyer is an international authority in glaucoma and neuro-ophthalmology. She is one of the most highly regarded experts in her field, having published more than 120 articles.