Ischaemic optic neuropathy or retinal artery occlusion?
An 82-year-old male patient was referred to the neuro-ophthalmology clinic with a history of decreased vision in the lower half of the left eye (LE) for the last six months, which was accidentally discovered when he covered his right eye. He was presumed to have had non-arteritic anterior ischaemic optic neuropathy (NAAION).
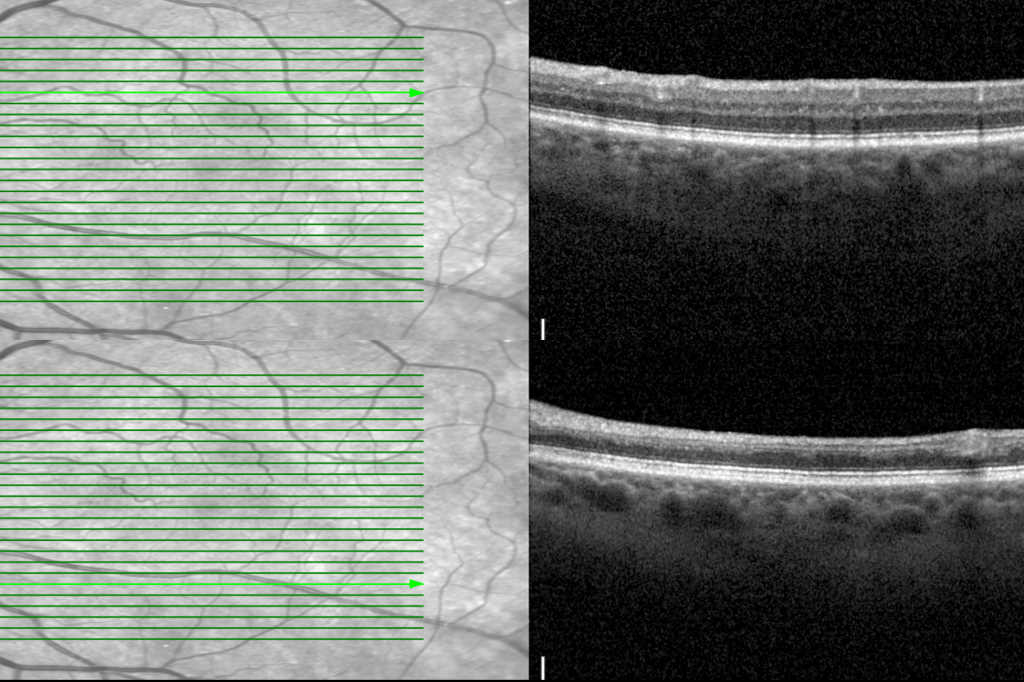
Visual acuity was 6/9 and 6/12 in the right and left eyes, respectively. He was pseudophakic and intraocular pressure was normal. The posterior segment examination of LE showed inferior sectoral pallor of the optic disc. The rest of the retinal examination was normal. Visual field assessment showed a superior altitudinal defect (Fig 1), and thinning of the retinal nerve fibre (Fig 2). Ganglion cell layer (GCL) was also noted (Fig 2). Systemic history included hypertension, dyslipidaemia and ischaemic heart disease, which had necessitated cardiac surgery.

Fig 1. Top: OCT shows thinning of inferior RNFL. Bottom left: HVF of the left eye showing
altitudinal field defect. Bottom right: OCT of the LE. Top demonstrates normal thickness
of inner retinal layers superior to the fovea; bottom reveals marked thinning of the inner
retinal layers inferior to the fovea

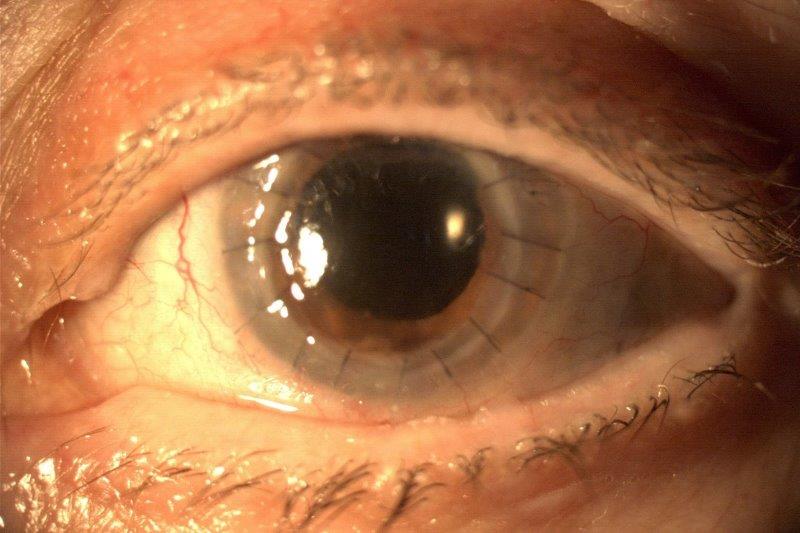
Fig 2. Top: typical full thickness scan and ganglion layer cell layer scan in a patient with
NAAION. Bottom: full thickness scan and ganglion cell layer scan in this patient. Note the
marked decrease in the full retinal thickness in contrast to a patient with NAAION
Despite the suspicion of NAAION, a careful evaluation of OCT scans showed thinning inner layers of the retina inferior to the fovea (Fig 1). Segmentation of the retinal layers showed reduced thickness of the retina and thinning of the ganglion cell layer, inner nuclear and outer plexiform layers inferior to the fovea. (Fig 2 and 3).

Fig 3. Top: typical inner nuclear and outer plexiform cell layer scan in a patient with
NAAION. There is no difference noted in the superior and inferior half. Bottom: inner
nuclear and outer plexiform cell layer scan in this patient. Note: the marked decrease in
inferior half compared to the upper half
Therefore, a diagnosis of an inferior branch retinal artery occlusion (BRAO) was made instead. He was referred to the stroke team for assessment of risk factors and was started on a combination of anti-platelets (aspirin and clopidogrel) to reduce the risk of stroke. Further investigations revealed left carotid stenosis of 80%, for which he underwent carotid endarterectomy.
Discussion
This case highlights the potential for occult branch retinal artery occlusion (BRAO) to mimic and be misdiagnosed as NAAION, as well as the diagnostic utility of segmented spectral-domain optical coherence tomography (SD-OCT) macular scans to differentiate between the two conditions.
The retina has dual blood supplies, with inner retinal layers supplied by the retinal vascular system, while the outer layers are supplied by the choroidal vascular system. Although outer plexiform is the watershed zone, it is mostly supplied by the retinal arterial system. Hence, it can be expected that all the inner retinal layers up to the outer plexiform will show structural changes in patients with retinal arterial occlusion.
Both BRAO and NAAION share common risk factors, including advancing age, male sex, smoking, hypertension, dyslipidaemia, diabetes, coronary artery disease, stroke, atrial fibrillation and hypercoagulability1-3. Both these conditions present similarly in the acute phase with painless acute vision loss and are easy to differentiate with very distinctive clinical features. However, in the late phase it becomes increasingly difficult to distinguish one from the other, as was illustrated in this case.
In the setting of occult BRAO, patients may present following the resolution of acute phase clinical signs, including localised opaque inner retinal oedema, and there might also be a reversal of delayed focal retinal artery filling and arteriovenous transit time on fundus fluorescein angiography, secondary to partial canalisation of the previously occluded artery4. Hence, it is not uncommon to overlook the diagnosis of occult BRAO.
In the late phase, both of these clinical conditions can have similar clinical features, namely altitudinal visual field defect, sectoral optic disc pallor and reduced thickness of retinal nerve fibre and ganglion cell layer5. Telltale retinal signs of arterial occlusion are often not visible. As illustrated in the current case, segmented SD-OCT macular scans can be useful for differentiating between occult BRAO and NAAION.
Long-term structural changes of the inner retinal layers within the vascular territory of the BRAO have been reported to cause prominent atrophy and thinning of the inner nuclear, inner plexiform, ganglion cell and retinal nerve fibre layers, as revealed by OCT macular scans6,7. In contrast, sectoral disruption of the vascular supply of the optic nerve head in NAAION leads to retrograde degeneration and corresponding thinning and atrophy, which is typically limited to the ganglion cell and retinal nerve fibre layers in OCT macular scans, with relative preservation and sparing of the inner nuclear and outer plexiform layers6.
The accurate distinction between occult BRAO and NAAION is clinically significant. In particular, the diagnosis of occult BRAO necessitates a careful investigation of the potential underlying cardioembolic or atherosclerotic causes of vascular occlusion to reduce the risk of serious systemic vascular occlusive events such as stroke or myocardial infarction2. Indeed, a previous meta-analysis reported the incidence of acute cerebral ischaemia was 25% among patients with BRAO8.
In conclusion, occult BRAO and NAAION can present similarly and be potentially subject to misdiagnosis. Segmented SD-OCT macular scans can be a useful diagnostic tool to assist with the differentiation of the two conditions. A profound reduction in the total thickness of the retina can provide an important clue to look for a vascular cause in the absence of the ability to segment all the inner retinal layers individually.
References
1. Callizo J, Feltgen N, Pantenburg S, et al. Cardiovascular Risk Factors in Central Retinal Artery Occlusion: Results of a Prospective and Standardized Medical Examination. Ophthalmology. 2015;122(9):1881-1888.
2. Hayreh S. Acute retinal arterial occlusive disorders. Prog Retin Eye Res. 2011;30(5):359-394.
3. Cestari D, Gaier E, Bouzika P, et al. Demographic, Systemic, and Ocular Factors Associated with Nonarteritic Anterior Ischaemic Optic Neuropathy. Ophthalmology. 2016;123(12):2446-2455.
4. Sullivan-Mee M, Amin P, Pensyl D, Katiyar S. Differentiating Occult Branch Retinal Artery Occlusion from Primary Open-angle Glaucoma. Optom Vis Sci. 2018;95(2):106-112.
5. Hayreh S, Zimmerman B. Visual field abnormalities in nonarteritic anterior ischaemic optic neuropathy: their pattern and prevalence at initial examination. Arch Ophthalmol. 2005;123(11):1554-1562.
6. Ghazi N, Tilton E, Patel B, Knape R, Newman S. Comparison of macular optical coherence tomography findings between postacute retinal artery occlusion and nonacute optic neuropathy. Retina. 2010;30(4):578-585.
7. Shetty R, Boilling J, Stewart M, Heckman M. Differences in optical coherence tomography of the macula in advanced glaucoma and after a retinal artery occlusion. Ophthalmic Surg Lasers Imaging. 2007;38(5):392-398.
8. Fallico M, Lotery A, Longo A, et al. Risk of acute stroke in patients with retinal artery occlusion: a systematic review and meta-analysis. Eye (Lond). 2020;34(4):683-689.

Dr Arvind Gupta is a consultant ophthalmologist specialising in cataract, medical retina and neuro-ophthalmology. He is based at Manukau Super Clinic, Greenlane Clinical Centre and Eye Doctors in Auckland.