SCHS approves MIGS, artificial irises
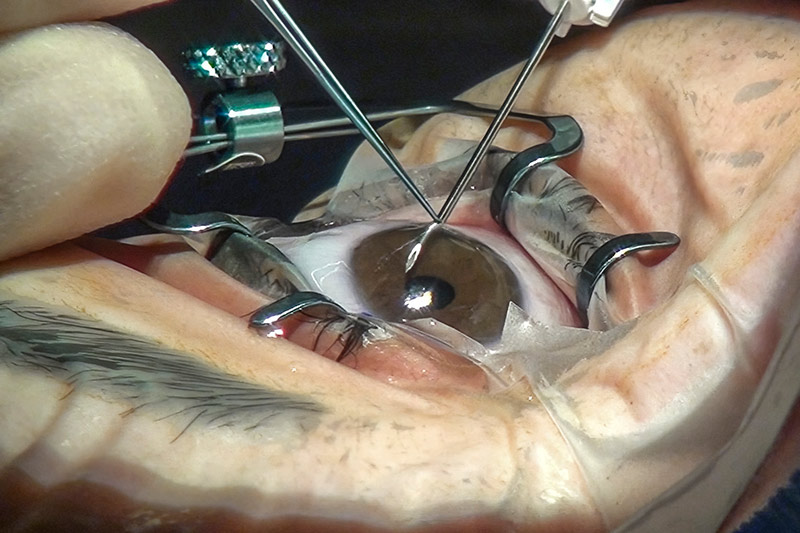
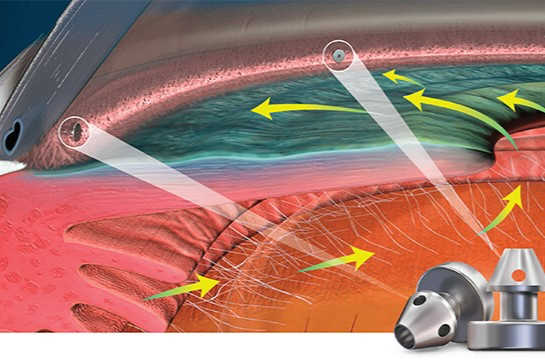
After more than five years and four applications, New Zealand’s largest private insurer, Southern Cross Health Society (SCHS) has added minimally invasive glaucoma surgery (MIGS) devices to its members’ policies.
The long-awaited policy change came about after several meetings with Ophthalmology New Zealand (ONZ) and because the financials finally made sense, said Dr Stephen Child, SCHS’s chief medical officer. Clinical efficacy has never been an issue with MIGS, said Dr Child, it’s always been about cost, affordability and benefit to members when compared with the many other medical products and procedures vying for approval. Given the definition of what constitutes a MIGS device or procedure is quite broad and can be quite fluid, it’s also quite a complex issue, he said. “It’s been really hard to write a business case when it's so kind of nebulous: what is MIGS, what is not MIGS, how are we going to price this, what's the volume going to be?”
To address these issues and allow flexibility in provider-patient choice, SCHS’s new MIGS policy covers all MIGS devices and procedures, however defined, said Dr Child, but the procedure and device will be charged separately. The procedure will be contracted via SCHS’s Affiliated Provider (AP) agreements, individually brokered with each ophthalmologist and roughly based on rates for similar surgeries, such as vitrectomy, he said. About 68% of all SCHS claims are paid through AP contracting, with contracts calculated at the 66th percentile, said Dr Child. “In other words, we offer basically what 66% of them have been charging, or higher. Everyone won’t be happy, but it's a negotiation. The majority, though, I think will be happy.”
The MIGS devices will be split into three price brackets or ‘prosthesis limits’, based on what the suppliers charge for their products and what SCHS has paid in the past. “There’s been a few MIGS procedures that have come through under fees-for-service - through back doors - so we’ve got some data, plus we've spoken to the companies, and ONZ has helped us. We're going to pay up to this amount for each device and then a member can pay the difference.”
Though SCHS doesn’t allow ‘top-ups’ for procedures, members can pay extra for prostheses. “But obviously we’ve picked these prosthesis limits at what we think is reasonable,” said Dr Child, stressing the rates are carefully worked out to be as fair as possible to members.
Both ONZ chair Dr Dean Corbett and MIGS manufacturer Glaukos welcomed the policy change. “Glaukos welcomes the news that a large proportion of patients with private healthcare will now have better access and funding for sight-saving devices like iStent inject W,” said Glenn Fawcett, Glaukos vice president Asia Pacific. “This was achieved by the substantial body of clinical evidence on iStent technologies, along with advocacy from Glaucoma New Zealand and the ongoing dedication and work by ophthalmologists in New Zealand to address the needs of patients with glaucoma.”
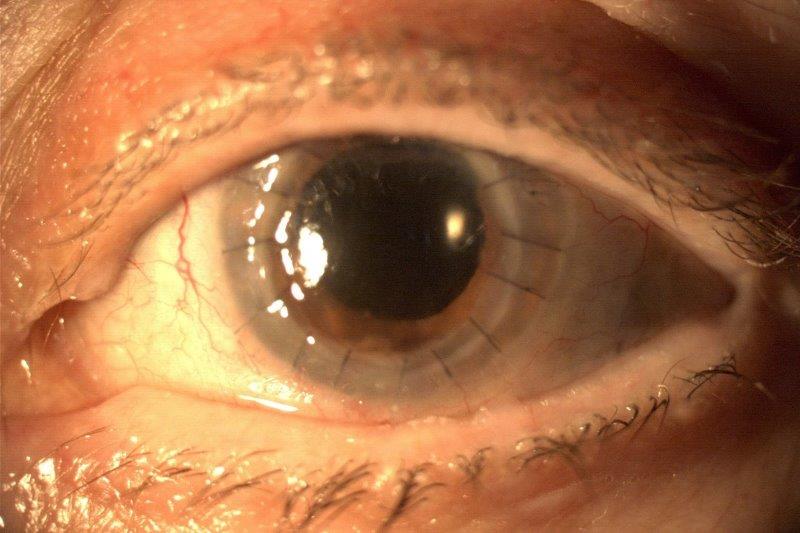
SCHS has also approved cover for prosthetic iris devices, bypassing its own veto on ‘custom-made’ prostheses since artificial irises need to be customised to match a patient’s eye colouring. This is likely to be charged in the same way as MIGS, said Dr Child, but the detail is still being worked out.
Dr Corbett said he was delighted to hear of the MIGS and the artificial iris implant approvals, both essential therapeutic surgical tools to address significant ocular pathology. “ONZ has been progressing this issue for its members and their patients for a number of years now.” ONZ would, however, have preferred an open negotiation with SCHS on behalf of all its members on the intended reimbursements, he said. “Using the AP system, in our view, may not provide the ability to deliver equity of access to care for patients across different providers, especially where there is no mechanism to offset real expenses that clinicians have had to absorb over recent years. We look forward to reviewing the process of negotiations SCHS has with our members.”
The artificial iris approval is excellent news, said corneal disease specialist Professor Charles McGhee, head of ophthalmology at the University of Auckland, especially for patients who’ve had to endure iris tumour surgery. “Rigid intracapsular iris segments on CTRs (capsular tension rings) are now generally becoming obsolete, with the flexible artificial prosthetic iris placed either in the bag, in the sulcus or sutured to the sclera having become the standard of care internationally. It is great that Kiwis insured with Southern Cross will now have more ready access to this transformative prosthesis, which has been available in the public service for the last five years.”
SCHS plans to contact ophthalmologists in December to start the contracting process and start funding MIGS and iris prostheses in early 2024, said Dr Child. “I'm a clinician as well, so it still blows my mind how long these things take. But we’re a $1.4 billion company now, with a million members. We have strict rules as a Friendly Society and we’re part of the CoFi (Conduct of Financial Institutions) regulations now, so we’ve got to do everything by the book, and it takes a long time!”