A rare but profound cause of corneal thinning
A 37-year-old male was noted to have decreased visual acuity (VA) in his left eye during a routine optometry exam. His previous medical and ocular history was otherwise unremarkable, with no significant family medical history of relevant systemic or ocular disease. On examination, the right eye appeared entirely normal; however, advanced, superior, peripheral, annular, corneal thinning with a high degree of against-the-rule astigmatism was identified in the left eye. A working diagnosis of Terrien’s marginal corneal degeneration (TMD) was confirmed oculus sinister (OS) by referral to an ophthalmologist with fellowship training in cornea and anterior segment disease.
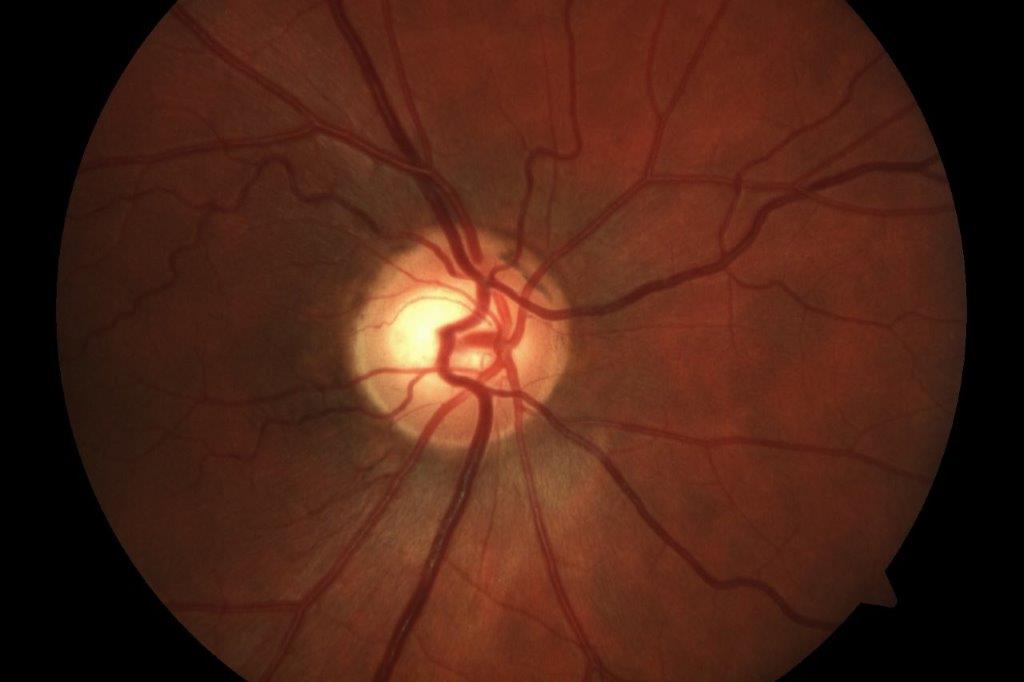
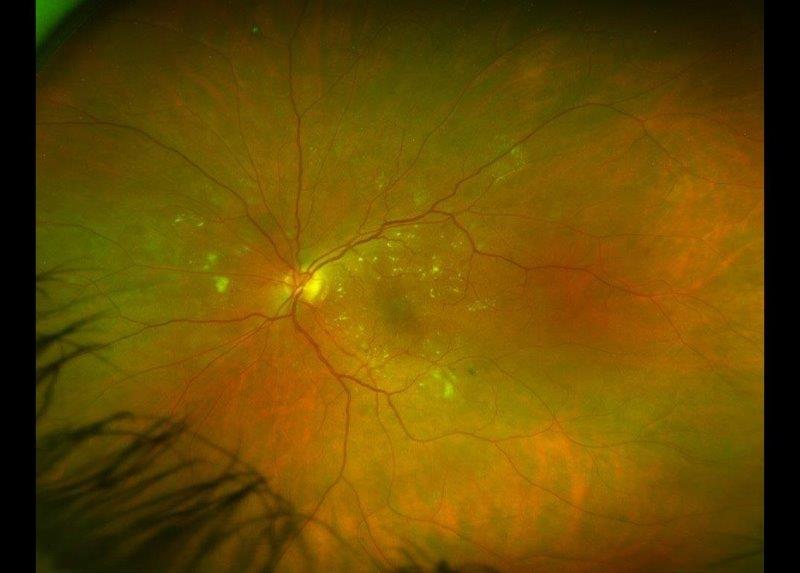
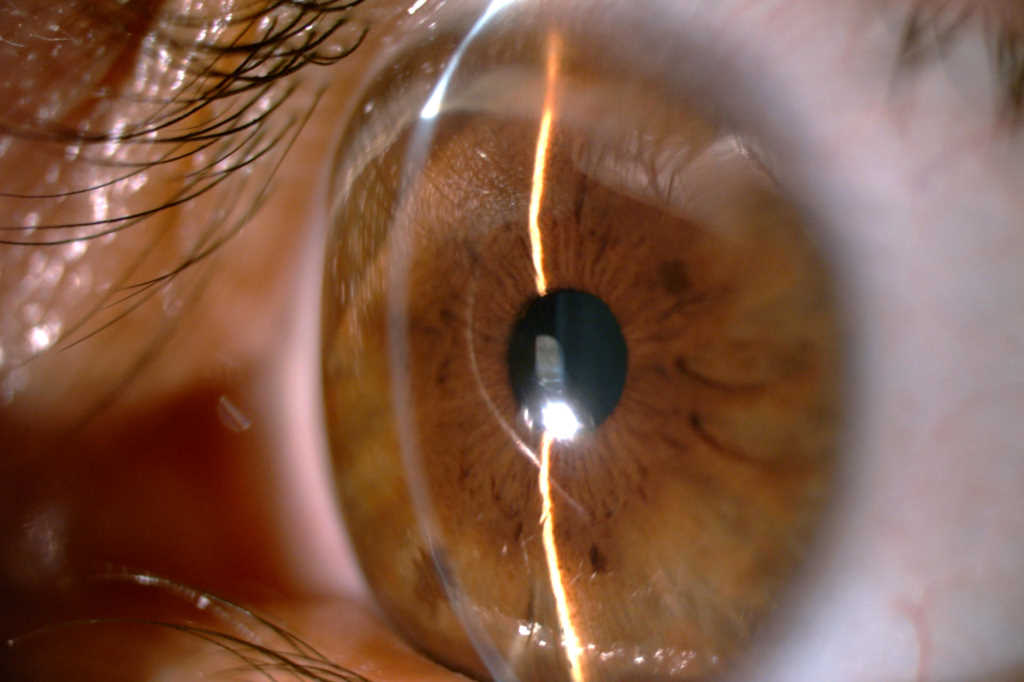
Since the diagnosis six years ago, his right eye has remained stable, with a best corrected visual acuity (BCVA) of 6/5 and no signs of TMD. However, the TMD in his left eye has progressed with his BCVA decreasing from 6/38 to counting fingers (6/45 with pinhole). On examination of his left eye, marked superior peripheral corneal thinning (Fig 1), with vascularisation, intact epithelium and a ‘wave’ of lipid deposition was noted (Fig 2). There was no fluorescein staining and the anterior chamber was quiet. The patient reported occasional, intermittent ocular surface inflammation, which was managed with topical corticosteroid drops, typically fluorometholone 0.1%.
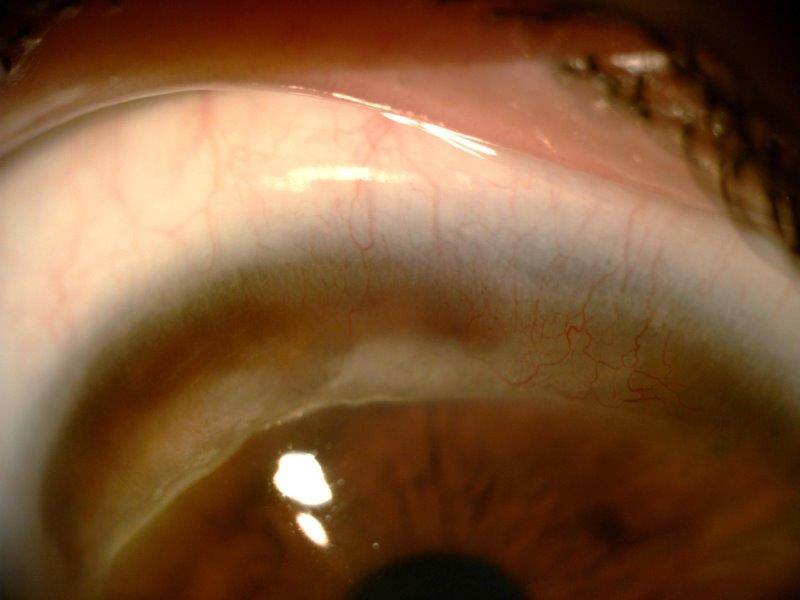
Fig 2. On higher magnification and visualised with diffuse light, localised superficial vascularisation can be seen over the area of corneal thinning as well as a ‘wave’ of lipid deposition in the leading edge, as observed in this patient with TMD
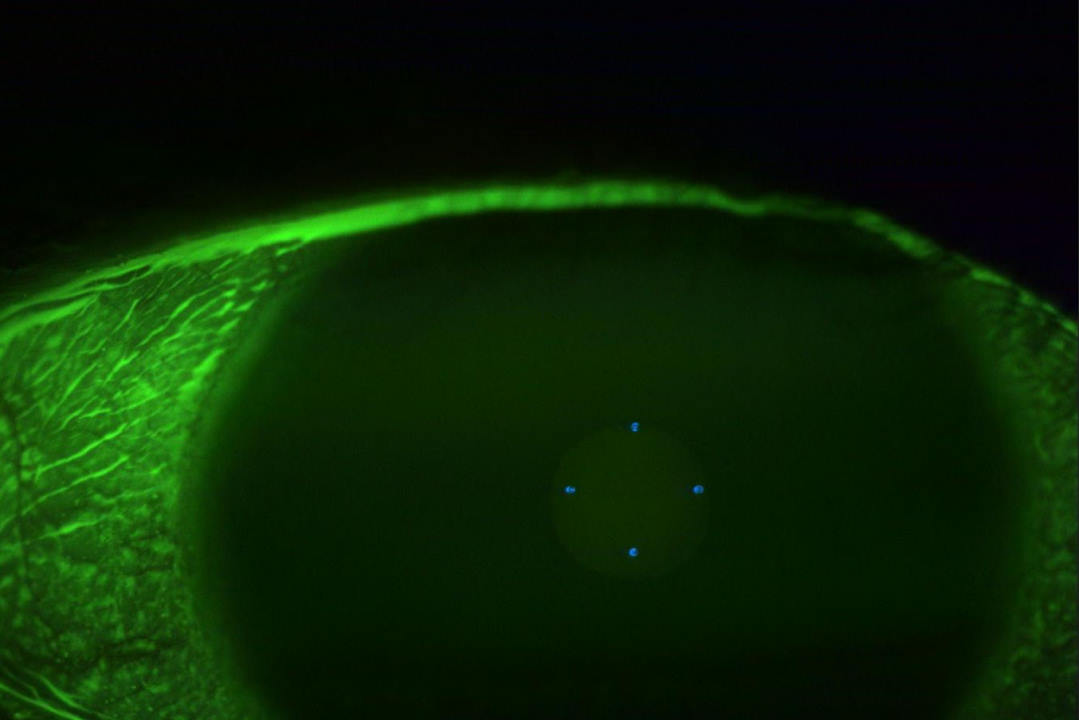
Further investigations, including anterior segment optical coherence tomography (OCT), confirmed significant thinning and anterior bulging of the corneal curvature superiorly, with the thinnest area measuring 120µm (Fig 3). The remainder of his cornea, beyond the peripheral zone of thinning, was slightly thicker than normal (651µm). Corneal topography showed corneal astigmatism of 16.52D (K1: 35.42D @113°, K2: 51.94D @23°). Due to the slowly progressive nature of TMD in this case, the patient has been managed conservatively; however, progressive thinning at his recent review prompted a discussion on elective surgical management with local excision of the affected tissue, followed by either a partial or full thickness graft, or use of a 180° annular (banana-shaped) graft.
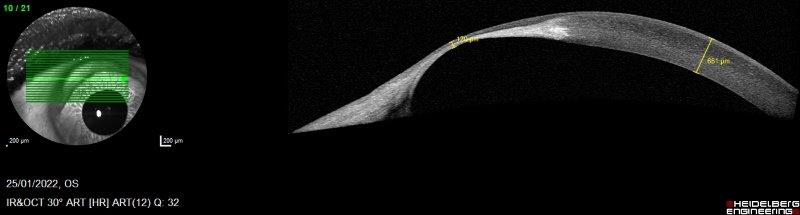
Fig 3. An anterior segment OCT snapshot over the thinnest area of the cornea affected by TMD. The thinnest portion of the cornea is 120μm, compared to the patient’s cornea elsewhere, measuring 651μm
Discussion
This case includes a classical clinical history, examination findings and OCT changes seen in an uncommon but very distinct form of marginal thinning of the cornea known as Terrien’s marginal degeneration. TMD is a rare, idiopathic and often bilateral but asymmetric disease of the cornea that generally presents with a painless, slowly progressing blurring of vision1. Being a rare disease, no prevalence or incidence data have been documented in the literature1. Historically, TMD was noted to affect middle-aged males2; however, a 2015 cross-sectional study demonstrates no evidence that it affects males more than females, and that it can commence at almost any age2,3.
The diagnosis of TMD is typically clinical and involves ruling out other peripheral corneal thinning disorders such as Mooren ulcer, peripheral ulcerative keratitis, peripheral microbial keratitis, Fuchs’ superficial marginal keratitis, dellen or pellucid marginal degeneration. Unlike TMD, which is painless, most other differential diagnoses present with ocular pain, photophobia, and/or lacrimation. Common findings in establishing the diagnosis of TMD include an intact corneal epithelium with peripheral (typically superior or supero-nasal) corneal thinning, lipid deposits at the leading edge alongside a steep central edge, superficial limbal vascularisation over the thinned cornea and conjunctival hyperaemia without other inflammatory findings3. The thinning spreads circumferentially in a crescent-shaped fashion, similar to a Mooren ulcer, but TMD does not progress centrally and the central edge is not undermined. Questions have been raised in the literature about the presence of an inflammatory subtype of TMD, presenting with recurrent ocular pain, conjunctival hyperaemia, epiphora and photophobia1. However, consensus to date suggests that the described symptoms and clinical findings are attributable to concurrent episcleritis1 or other associated corneal or systemic diseases rather than a direct result of TMD itself2.
In TMD, the corneal thinning commonly starts superiorly or supero-nasally, resulting in a local flattening of the cornea1. Subsequently, relative steepening of the meridian perpendicular to the meridian that has thinned, produces significant against-the-rule astigmatism (up to 30D), which decreases visual acuity3. While progression is typically slow, it varies markedly from case to case, so regular follow-up is recommended3. With increased thinning, the risk of corneal perforation increases. Rates of perforation (both spontaneous and traumatic) are around 10-15%1 and are associated with poor visual outcomes even with prompt repair1. Because of this, education on the need for caution – and in advanced cases, protective eyewear – should be provided to TMD patients2.
Anterior segment OCT is a useful monitoring tool as it provides high-definition cross-sectional images of the cornea, allowing the thinning to be visualised and measured. In 2015, a new staging system was proposed based on OCT findings including: 1) anterior and posterior corneal curvature, and 2) thickness of the thinnest part of the cornea4. This provides an objective way to document progression of TMD and allows for better surgical planning and therefore prevention of perforation than the previous Süveges classification, which was based mainly on the width of the corneal lesion4.
In summary, the aetiology of TMD is unknown and there is no evidence that pharmacological therapies can halt its progression1, with surveillance and conservative management adequate for most patients2. Vision can be significantly improved in the early stages with corrective spectacles, or as the disease progresses with rigid gas-permeable contact lenses1. Surgical treatment is typically reserved for severe thinning (<150µm) where there is an increased perforation risk or where astigmatism severely limits VA2. Surgical treatment typically involves penetrating keratoplasty or lamellar keratoplasty, with the latter utilising a graft tailored to the shape and depth of the affected area, currently favoured2. While surgical treatment should not be undertaken unnecessarily, surgery should be advocated earlier rather than later in advanced cases, to preserve corneal integrity and to avoid perforation.
Declaration of patient consent
The patient consented to his anonymised images and clinical information being used in this case report.
Acknowledgment
We thank Professor Charles McGhee for identifying this case from his practice and providing critical manuscript review.
References
1. Ding Y, Murri MS, Birdsong OC, Ronquillo Y, Moshirfar M. Terrien marginal degeneration. Surv Ophthalmol 2019;64(2):162-174.
2. Chan AT, Ulate R, Goldich Y, Rootman DS, Chan CC. Terrien Marginal Degeneration: Clinical Characteristics and Outcomes. Am J Ophthalmol 2015;160(5):867-872.e1.
3. Ruutila M, Fagerholm P, Lagali N, Hjortdal J, Bram T, Moilanen J, et al. Diagnostic Criteria for Terrien Marginal Degeneration: Nordic Terrien Degeneration Study. Cornea 2021;40(2).
4. Wang N, Wang C, Lian X, Duan S, Huang D, Zhou S. Staging of development in Terrien’s degeneration based on corneal curvatures detected by optical coherence tomography. Graefe's Archive for Clinical and Experimental Ophthalmology 2015;253(10):1757-1764.

Stephanie Townend (Te Kapotai) is a final-year medical student at the University of Auckland with a special interest in ophthalmology.

Dr Joevy Lim is a junior research fellow in Auckland University’s Department of Ophthalmology and a PhD candidate supported by an HRC Clinical Research Training Fellowship

Dr Simone Freundlich (Tainui, Ngā Puhi) is an ophthalmology trainee with an interest in cornea and anterior segment pathology, currently completing her second year at Dunedin Public Hospital.