OTE4 – Doing it for the kids
The final Ocular Therapeutics Evening (OTE) of the University of Auckland’s Buchanan Ocular Therapeutics Unit (BOTU) series was held online and focused on paediatric eyecare.
Dr Rasha Altaie, a paediatric ophthalmologist working in Counties Manukau and Milford Eye Clinic, discussed the use of low-dose atropine for paediatric myopia control, explaining that myopic eyes’ longer axial length means the sclera is thinner and more susceptible to vascular leakage. Research has shown that atropine has a dose-dependent effect on modulating choroidal thickness which retards the increase in axial length, she said. The recently published two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study (Yam et al, 2021) reported significant choroidal thickening in groups using 0.05% and 0.025% atropine, but this was not found in the 0.01% or placebo groups. The study also showed the choroid-thickening effect induced was maintained throughout the treatment period and that every 10µm of thickening was associated with 0.074D of spherical equivalent progression and 0.045mm of axial length elongation.
Other questions abound, including why 10% of children’s myopia progresses rapidly despite high-dose atropine use; why certain groups are less responsive to atropine than others; and what’s the extent of myopia progression reduction possible with atropine drops? A poorer response, however, has been associated with younger age children, a higher degree of myopia at baseline, children who started wearing spectacles younger and a history of parental myopia. Although there are some long-term side effects of topical atropine, such as photophobia and allergic conjunctivitis (due to the preservatives in the drops), the benefits of treatment largely outweigh these and there are no reports of related systemic adverse events. Dr Altaie advised, however, that long-term atropine use should be undertaken with caution since side effects have not been fully evaluated and that dosage or dose frequency should be tapered towards the end of the treatment to minimise rebound effects.
Ortho-k pros and cons
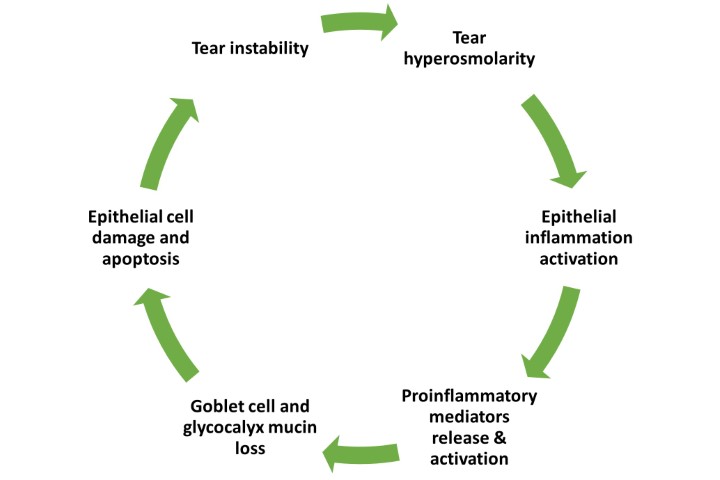
Optometrist Grant Watters shared his experience in orthokeratology (ortho-k) lenses for myopia control. Having only seen one case of microbial keratitis (MK) associated with ortho-k in his clinic, and noting that only one of 78 cases of contact lens-related keratitis was associated with ortho-k in a recent audit at Greenlane Acute Eye Clinic, Watters concluded that ortho-k-associated MK prevalence is very low in New Zealand. Ortho-k is associated with reduced non-invasive tear break-up time, increased corneal fluorescein staining, increased meibomian gland dysfunction scores and increased ocular surface inflammatory cytokines. However, the causal effect of ortho-k wear on atrophy of upper meibomian glands is still controversial, he said.

Grant Watters
Dr Cheefoong Chong, a consultant ophthalmologist at Tauranga Eye Specialists, the Waikato District Health Board (DHB) and Auckland DHB, discussed the treatment of children with retinoblastoma (RB). RB is the most common malignant childhood intraocular tumour of genetic origin and is found in approximately 1 in 15,000 live births globally. Since a parent with RB has a 50% chance of passing it to their offspring, it is very important to take a thorough family history when examining young children and note if anyone in the family is bi- or unilaterally blind. Early diagnosis means smaller tumours, which usually respond well to treatment, avoiding enucleation. While leukocoria (white pupil) is the most common sign of RB, it can be easily missed in red-reflex tests. Dr Chong advises learning and using the photoRED technique, where you turn off all lights in a room, turn off the red-eye reduction on your phone camera, stand 4m from the child and take photos from different angles, and then teach it to parents. The Cradle white-eye detector app is also a useful tool for parents to check the red reflex at home. While early identified cases of RB respond very well to laser treatment, vitreous cloud and vitreous seeds can still develop, making it difficult to treat with conventional chemotherapy because the vitreous is avascular, he said.
A holistic approach to blindness
Paediatric optometrist Dr Samantha Simkin focused on the impact of childhood blindness and best care for the patient and their family. While blind children only account for 4% of global blindness, they generally have a much longer life expectancy. It is also important to recognise that since good vision is vital for learning, children with low vision and blindness often experience developmental delay, physical disability, epilepsy and hearing impairment, she said. Though a large proportion of blind children have not received or are unsuitable for ophthalmic surgery, there are other support systems which can help them including the Blind and Low Vision Education Network NZ (BLENNZ), Blind Low Vision NZ and Parents of Vision Impaired. There are also disease-specific entities such as Albinism NZ and specialist therapists. It is important to provide ongoing support and education for the entire family, stressed Dr Simkin, and to refer low vision and blind children when we identify systemic associations to optimise their development.

Dr Samantha Simkin
Ocular outliers
Auckland Eye and Auckland DHB ophthalmologist Dr Sarah Hull presented a series of rare cases among her paediatric patients. The first was a baby who presented with unilateral ptosis and a smaller pupil with lighter coloured iris on the same side. Dr Hull used a 4-10% cocaine eye drop in both eyes to diagnose Horner’s syndrome. It’s difficult to take measurements on babies, therefore therapeutic diagnosis and photo taking can be very helpful, she said. Another common pharmacological test for Horner’s, 0.5% apraclonidine (Iopidine), was not used due to the risk of apnoea and bradycardia in babies under two years old. In this case, Horner’s could be due to a damaged cervical sympathetic nerve at the neck following forceps delivery. Further investigations were also needed to eliminate risk of neuroblastoma, which can begin in utero.
The second case was an 11-year-old girl with three days of right-eye pain and double vision on upgaze. Upon examination, it was found that the eye had restricted elevation at abduction (when looking up to the left). Magnetic resonance imaging revealed an unusual case of Brown’s syndrome, which usually occurs in adults with arthritis or is congenital in children due to a tight tendon sheath that runs through the trochlea of the inferior oblique muscle. Avoiding steroids, which could have side effects in young children, Dr Hull prescribed a course of oral ibuprofen and the patient achieved almost full recovery after four weeks.
The third case was a six-year-old boy with a three-month history of sudden onset left esotropia with no preceding trauma, viral illness or headache, with good visual acuity (VA), full extraocular muscle motility, healthy fundi and no significant refractive error. This was diagnosed as acute non-accommodative esotropia and the patient was treated with a course of Botox to each medial rectus muscle. Botox injection has a similar success rate to strabismus surgery, but is a better choice due to shorter anaesthesia, being less expensive and affording a faster recovery.
The final case involved a five-year-old with abnormal-looking bilateral macula. Optical coherence tomography (OCT) revealed accumulated mass underneath the macula, while autofluorescence fundus photography showed a circular, pseudo-hypopyon-like mass over the macula. This was diagnosed as Best vitelliform macular dystrophy (BVMD), an inherited disorder caused by a lack of lipofuscin clearance in the retinal pigment epithelium, which can lead to thinning of the macula. When the child turned seven, the VA dropped to 6/30 in one eye that had a haemorrhage underneath the macula and OCT revealed a cord of vascular membrane had formed. The vision improved to 6/9 after intravitreal Avastin injections.
If you would like to know more about these topics, the recording and MCQ quiz of OTE4 is now available on www.botu.nz. While this was the last evening of the 2021-2022 OTE series, the one-day conference, covering several exciting ocular therapeutics topics will return in early 2023.

Charisse Kuo is a therapeutically qualified optometrist in the third year of her PhD at the University of Auckland. Her research involves the development of tissue-culture models using human donor retinas and choroids to explore the mechanisms behind sight-threatening diseases.