Contemporary surgical managment of iris tumours and reconstruction
In the human eye, the iris forms a diaphragm controlling the diameter of the pupil and therefore the amount of light reaching the retina1. The eye is diffraction-limited, thus by varying the pupil diameter, the iris assists in achieving maxium depth of focus, controlling light entry in bright and low-level conditions and reducing light scatter from crystallline lens abberations to maximise vision quality2. In acquired-iris defects, such as those resulting from trauma or surgical excision of iris lesions, vision quality and cosmesis can be adversely affected.
Iris tumours
Benign iris naevi and iris melanomas are the most common primary tumours of the iris3-5. Benign iris naevi account for 49-72% of all iris lesions, while iris melanomas account for only 2-5% of all uveal melanomas3. Though iris melanomas are the most common primary iris malignancies, occurrence is rare. Internationally, iris melanomas are reported in 0.02-0.08/100,000 Europeans per year. In New Zealand, the rate is slightly higher occuring in 0.09/100,000 Europeans per year4, 5, attributed to higher levels of solar UV-B radiation exposure.
Although the majority of iris lesions are benign and the risk of metastases from iris melanoma is low, definitive classification and management of iris tumours remains important yet contentious4, 6. After reviewing 631 cases with a 10-year minimum follow-up, Geisse and Robertson found that mixed cell melanomas had a higher metastatic rate (10.5%) compared with epithelioid (6.9%) and spindle B melanomas (2.6%)7. Notably, even benign iris lesions can result in signifcant damage and loss of function to neighbouring ocular structures, including the pupil, angle and crystalline lens, occasionally requiring surgical excision.
Iris surgery
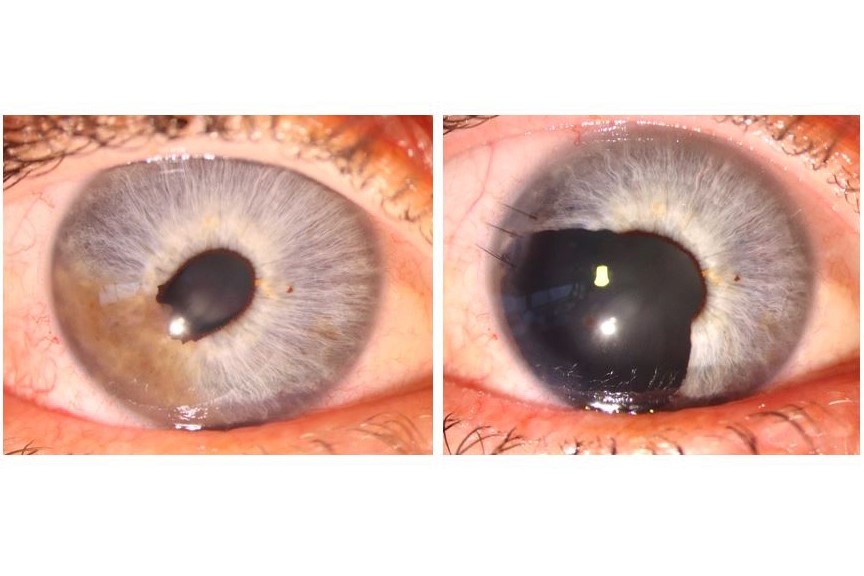
Surgical excision of an iris lesion and subsequent iris reconstruction requires multiple factors to be considered. One surgical method utilises a two-stage approach, involving minimal iris touch excision (MITE) of the iris lesion followed by delayed iris reconstruction, in conjunction with phacoemulsification and intraocular lens (IOL) insertion8, allowing time for histology review and planning to best-repair the iris defect (Fig 1) 9. Specifically, this enables consideration of patient vision and degree of glare/photophobia, cosmesis, size and position of iris defect and whether a primary iridoplasty repair with a small artificial iris segment in the bag, or a larger, colour-matched, iris replacement, is required.
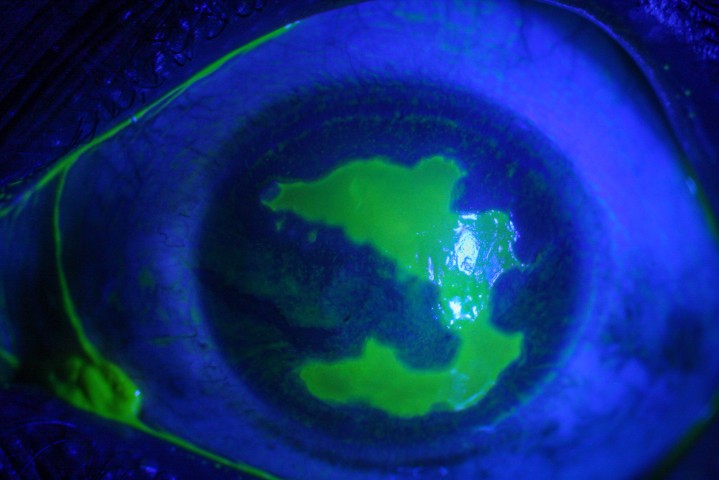
The MITE technique is a micro-incisional variation of sector iridectomy and involves complete excision of the circumscribed iris lesion with minimal trauma to both the iris specimen and remaining iris tissue8. In this technique surgical access is obtained through four, small 1.1mm paracentesis incisions. Two of the paracenteses enable radial incisions along the circumscribed tumour margins, while two are angled obliquely to allow peripheral excision of the iris at the iris root. The iris specimen is removed in an atraumatic fashion via a 2.7mm incision using an IOL insertor that enables the tumour to gently move up the inside of the insertor ‘tube’ by capillary action and thus be removed from the anterior chamber without damage to the specimen or contact with the corneal incision or the ocular surface (Fig 2) 8.
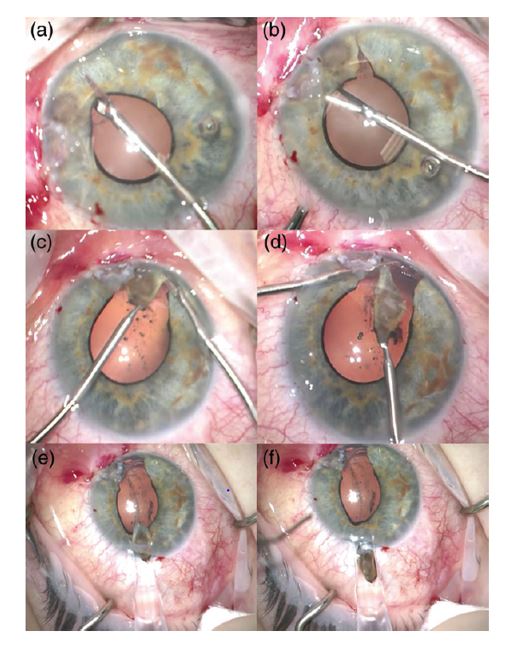
Fig 2. MITE procedure stages: A) first radial incision B) second radial incision C) first basal iris incision D) second basal iris incision (all incisions via 1.1mm paracenteses using micro-scissors and forceps) to free iris tumour. An IOL cartridge is inserted into the anterior chamber via 2.7mm incision (E) and the tumour moves up the tube and is removed (E & F) without trauma to the specimen or contact with the corneal incision or ocular surface⁸.
Following tumour excision, surgical iris reconstruction can be achieved through 1) minimally invasive pupilloplasty, 2) partial aniridia segment ring with or without pupilloplasty or 3) a full artificial iris implant. These approaches are performed in conjunction with planned cataract surgery if required. Minimally invasive pupilloplasty, performed using an iris suture passed through two corneal paracentesis incisions, was introduced by McCannel in 1976. However, the technique has evolved to be performed under viscoelastic with the use of a locking slip knot to reduce the risk of suture failure10, 11. While technically challenging, this approach can achieve satisfactory results in reforming the pupil shape, reducing the size of the iris defect and the associated symptoms. Limitations of pupilloplasty include excessive intraoperative manipulation or iris traction, precipitating further iris damage or repair failure11; inability to restore the pupil sufficiently to reduce glare or dysphotopsia; and unsatisfactory cosmesis.
Iris defect repair can also be achieved through insertion of an iris segment such as a Morcher partial aniridia ring placed in the capsular bag (Fig 3A). This is suitable for defects that extend between 90-180 degrees12. The intracapsular partial aniridia ring (IPAR) is composed of polymethyl methacrylate (PMMA), with a diameter of 10-11mm when compressed and contains a single ‘fin’ segment12, 13. Insertion of the device requires >3.5mm corneal incision. In the presence of good capsular support, the partial aniridia ring can be placed “in the bag” following IOL posititioning. In pseudophakic eyes, a partial aniridia ring may still be postioned in the bag following careful visco-dissection to re-open the capsular bag12. In larger iris defects, the segment fins of two IPARs can be placed side by side to accomodate a defect of up to 180 degrees or pupilloplasty may be performed where possible to achieve the greatest coverage (Fig 3B and 3C). Endo-capsular positioning of the IPAR avoids contact with the ciliary body and angle structures, minimising postoperative inflammation and reducing the risk of uveitis-glaucoma-hyphaema (UGH) syndrome12. The main limitations of IPARs include a slightly larger incision size compared to more conservative approaches, the black appearance of the segment in situ (although fibrosis of the overlying lens capsule renders this grey with time) and potential damage to the ring or capsule during insertion12. However, the IPAR approach can deal with significantly larger defects (up to 180 degrees) than the McCannel technique alone (around 90 degrees).
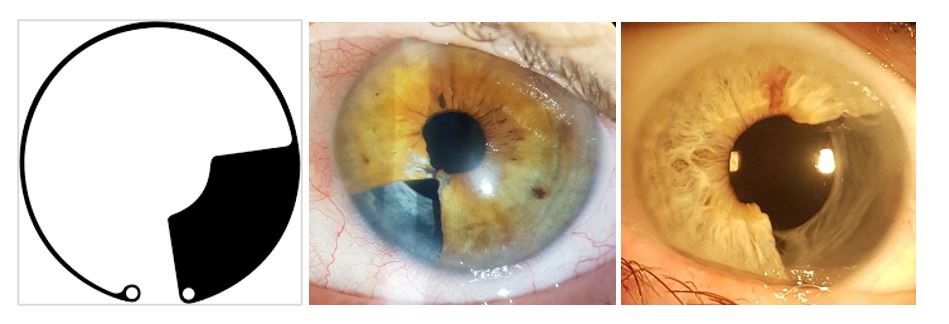
Fig 3. L-R: A) Morcher IPAR with a single 90⁰ segment for occlusion of iris defects; B) infero-nasal iris defect post-MITE reconstructed with a McCannel suture to pupil margin and one 90-degree black IPAR with IOL in capsular bag; C) a temporal, four-clock hour iris defect repaired with a black IPAR and IOL. Images B&C show grey-white fibrosis of lens capsule overlying IPAR, making the black IPAR less obvious
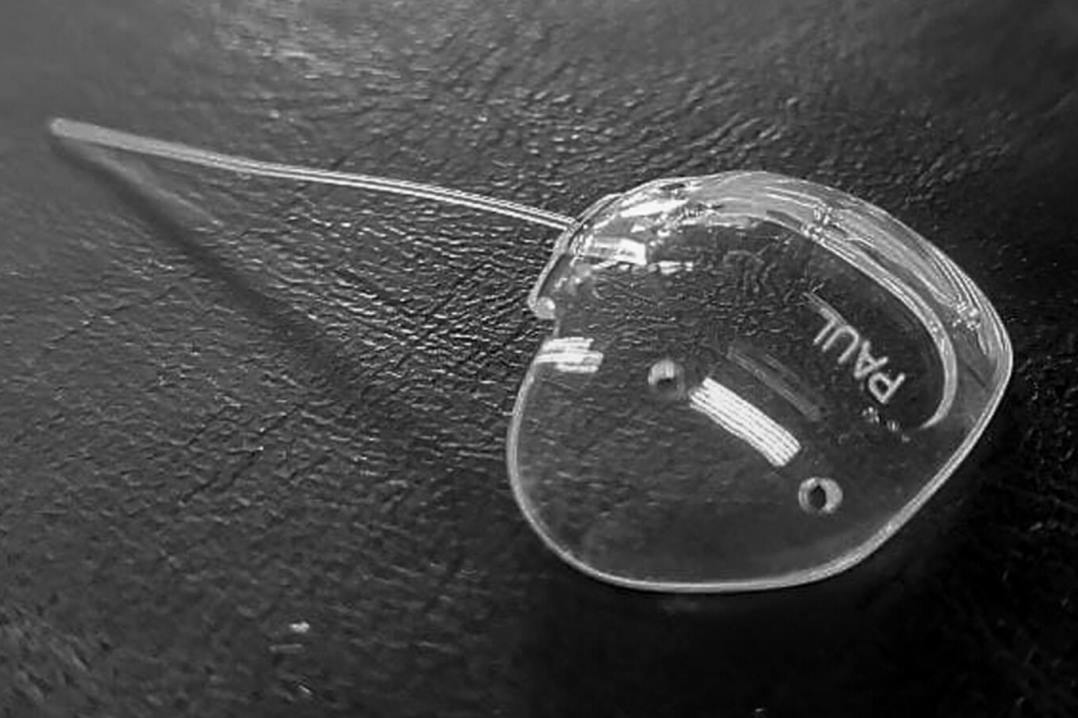
In larger iris defects reconstruction can be achieved with an artificial iris implant such as the Human Optics artificial iris9. This flexible silicone iris has a diameter of approximately 12.8mm with a fixed pupil aperture of 3.35mm14. The thickness of the iris decreases from the pupillary edge where it is 0.40mm to 0.25mm at the peripheral edge. The anterior surface of the iris is hand-crafted by the manufacturer using pigmented silicone based on the patient’s healthy contralateral eye. Prior to insertion, the artificial iris is trephined to a diameter appropriate for the patient’s capsular bag (or ciliary sulcus) depending on planned placement. In eyes with good zonular stability the artificial iris can be positioned in either the capsular bag following IOL positioning, or it can be placed in the sulcus with or without scleral sutures in eyes with zonular instability14.
Depending on the implantation technique, the incision for implantation of the Human Optics artificial iris ranges from approximately 3-7mm. Injector-assisted implantation following phacoemulsification surgery uses an approximate 2.7mm incision. It is important to ensure that the endothelium is well protected through the use of viscoelastic as the iris unfolds14. Postoperative shrinking of the capsular bag whilst rare, may result in tilting or displacement of the iris. This may be prevented through the insertion of a capsular tension ring at the time of surgery14. Benefits of the artificial iris include excellent cosmesis (Fig 4) and when positioned in the capsular bag complications are reportedly similar to those of IOL’s14.
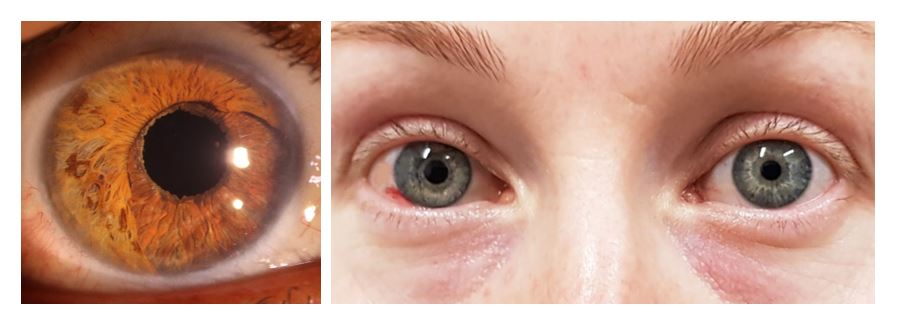
Fig 4. A) High power slit-lamp view of a HumanOptics artificial iris in a brown-eyed patient following wide excision of an iris melanoma. B) Artificial iris appearance following 5-clock hour nasal iris melanoma excision in right eye of blue-eyed patient, one day post-surgery
Postoperative follow-up of all three reconstructive techniques should include frequent review for assessment of visual acuity, intraocular pressure, implant positioning and inflammation/cystoid macular oedema14. Patient selection prior to surgery is also critically important. Patients with a greater risk of postoperative problems include those with a history of glaucoma, inflammation or low endothelial cell density14. Fortunately, post-operative complications are relatively uncommon where iris prostheses are placed in the capsular bag and patients typically achieve visual acuity in the region of 6/5 to 6/9. However, complications may be more common in those eyes that have suffered severe trauma and the iris/IOL complex needs to be sutured to the sclera. In the specific context of iris tumours, the patient undergoes iris reconstruction typically within three months of their initial procedure. As such, insertion of a capsular tension ring and an iris segment or artificial iris for a patient undergoing cataract phacoemulsification and IOL insertion may compromise the blood-eye-barrier placing the patient at greater risk of cystoid macular oedema.
Microsurgical techniques for the surgical management of iris tumours have advanced significantly in the last decade and these have been mirrored by dramatic improvements in iris reconstruction, as highlighted in this brief report. However, systemic workup and adjunctive techniques such as brachytherapy, radiotherapy or, rarely, chemotherapy, are still required in the minority of patients. Thus, following referral and investigation, the management of iris melanoma always requires a collaborative team approach involving anterior segment, vitreo-retinal, ocular oncology, radiotherapy and systemic oncology specialists.
References
- Srinivasan S, Ting DS, Snyder ME, Prasad S, Koch HR. Prosthetic iris devices. Can J Ophthalmol. 2014;49(1):6-17.
- Slomovits T L, Glaser J S. Tasman W, Jaeger E, eds. . In: Tasman W, E J, editors. Duane’s Clinical Ophthalmology 2013 Edition Philadelphia, Pa Lippincott Williams & Wilkins; 2013.
- Shields CL, Kancherla S, Patel J, Vijayvargiya P, Suriano MM, Kolbus E, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology. 2012;119(2):407-14.
- Michalova K, Clemett R, Dempster A, Evans J, Allardyce RA. Iris melanomas: are they more frequent in New Zealand? Br J Ophthalmol. 2001;85(1):4-5.
- Khan S, Finger PT, Yu GP, Razzaq L, Jager MJ, de Keizer RJ, et al. Clinical and pathologic characteristics of biopsy-proven iris melanoma: a multicenter international study. Arch Ophthalmol. 2012;130(1):57-64.
- Starr OD, Patel DV, Allen JP, McGhee CN. Iris melanoma: pathology, prognosis and surgical intervention. Clin Exp Ophthalmol. 2004;32(3):294-6.
- Geisse LJ, Robertson DM. Iris melanomas. Am J Ophthalmol. 1985;99(6):638-48.
- Meyer JJ, Krishnan T, McGhee CN. Minimal iris touch excision: a novel surgical technique for local excision of iris melanoma. Clin Exp Ophthalmol. 2018;46(3):298-9.
- Spitzer MS, Nessmann A, Wagner J, Yoeruek E, Bartz-Schmidt KU, Szurman P, et al. Customized humanoptics silicone iris prosthesis in eyes with posttraumatic iris loss: outcomes and complications. Acta Ophthalmol. 2016;94(3):301-6.
- Cionni RJ, Karatza EC, Osher RH, Shah M. Surgical technique for congenital iris coloboma repair. J Cataract Refract Surg. 2006;32(11):1913-6.
- Osher RH, Snyder ME, Cionni RJ. Modification of the Siepser slip-knot technique. J Cataract Refract Surg. 2005;31(6):1098-100.
- Srinivasan S, Yuen C, Watts M, Prasad S. Endocapsular iris reconstruction implants for acquired iris defects: a clinical study. Eye (Lond). 2007;21(8):1109-13.
- MORCHER. Morcher Ophthalmic Implants 2020 [cited 2020 25 Nov ]. Available from: https://www.morcher.com/nc/en/products/aniridia-implants.html.
- Mayer C, Tandogan T, Hoffmann AE, Khoramnia R. Artificial iris implantation in various iris defects and lens conditions. J Cataract Refract Surg. 2017;43(6):724-31.
Dr Simone Freundlich is the current Maurice and Phyllis Paykel corneal and anterior segment clinical research fellow at the Department of Ophthalmology, University of Auckland.
Professor Charles McGhee is chair of ophthalmology at Auckland University, director of the National Eye Centre and immediate past-president of the Asia Pacific Academy of Ophthalmology.