Influence of eyelid malposition on dry eye
The eyelids protect the eye physically, by blinking, which protects the ocular surface from noxious insult and facilitates tear spreading via secretion of lipids from the meibomian glands. Involutional or iatrogenic eyelid changes can influence eyelid function, potentially leading to dry eye. This results in tear hyper-evaporation that drives hyperosmolarity, accompanied by symptoms of irritation and variable vision as well as inflammation and epiphora.
Some simple surgical measures can help address lid malposition, helping to treat dry eye disease by restoring the lids to a more functional anatomical position, thereby reducing ongoing reliance on temporary symptomatic relief from drops.
Involutional eyelid changes
The combination of gravity and age is the key underlying aetiology in both upper- and lower-lid laxity. Upper-lid laxity offers greater eye protection in the setting of tear film instability by providing more shielding. However, the lids may droop to a point where they interfere with vision (dermatochalasis). In this setting, a blepharoplasty wouldn’t be expected to improve dry eye, but should be approached cautiously in the presence of significant tear film instability. The same applies to blepharoptosis (ptosis) surgery. It is important to respect the underlying globe and not induce lagophthalmos (inability to close the eyelids) when any upper lid lift is undertaken.
The lower lids are attached at each end like a clothesline so a normal lid position will not expose the inferior bulbar conjunctiva. However, with time and gravity the lids will droop and an early clinical sign of this is a slow snap-back test. Later this can deteriorate to display inferior scleral show. Lower-lid laxity exacerbates dry eye by impairing the blink and also increasing exposure. Paradoxically, patients often complain of intermittent epiphora with dry eye, and tear pooling and spillover are exacerbated by lower-lid laxity. Increasing laxity can progress to punctal ectropion (amplifying any drainage insufficiency) and possibly manifest ectropion or entropion. All of these should reduce with lateral traction unless there is an additional cicatricial component, for example rosacea or lower-lid blepharoplasty. A lateral horizontal lid tightening procedure for the lower lids, therefore, is typically helpful in the setting of dry eye and is relatively quick and easy to perform.
Iatrogenic eyelid changes
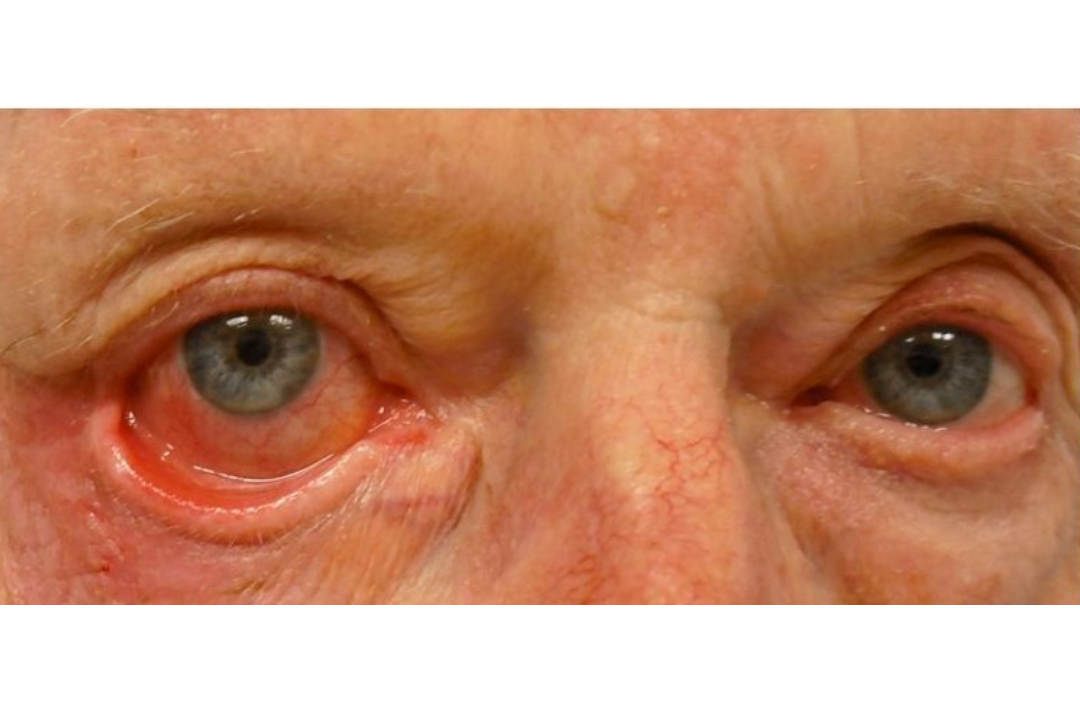
Exuberant upper- or lower-lid blepharoplasty or ptosis surgery can trigger or exacerbate tear film instability. Repeat blepharoplasty can present a further risk to tear film destabilisation. A simple lateral tarsorrhaphy to reduce exposure may be useful if this proves difficult to manage conservatively. Other frequently encountered causes of lagophthalmos include Bell’s palsy or 7th nerve palsy palsy, which could result from surgical intervention for an acoustic neuroma, for example. In this setting, surgery to reduce exposure may involve an upper-lid gold weight, to counteract the unopposed levator action, and a lower-lid tightening and deep support to lift the lid and cheek to minimise the neurogenic ectropion. A direct brow lift can help with uncovering the visual axis if there is significant brow ptosis (Fig 1).


Fig 1. (B) Surgical repair involved a direct brow lift, upper lid gold weight and lower-lid tightening. (C) By four weeks’ post-op dry eye and conjunctival redness are resolved due to anatomically restored lid position
Lid or periocular tumour excision may cause a cicatricial ectropion and there are ways to address this, ideally during the primary procedure but, potentially later, with rotation flaps, for example, to alter the direction of tension.
Mechanical and other ectropion
Benign lid masses may cause a mechanical ectropion. Debulking often helps. Trichiasis (independent of entropion) can be managed with a series of electrolysis sessions. Thyroid-related orbitopathy may result in exposure due to exophthalmos. Sometimes a simple lid-lowering procedure can be offered or, potentially, orbital decompression if severe and associated with diplopia. Punctal plugs or cautery may also be useful when there’s significant aqueous deficiency, such as in Sjögren syndrome.
Summary
In the setting of dry eye, it’s helpful to understand eyelid function and how surgery has potential to both exacerbate and address dry eye issues. While hot lid compresses to improve lipid quantity and quality is the mainstay of dry eye management, certainly it is worth assessing lower-lid laxity (inferior scleral show) to see if lower-lid tightening could be useful.
With the eyelids being a critical component of the lacrimal functional unit that maintains ocular surface integrity, an oculoplastic surgeon may be able to help address lid malposition issues where they are present within an often multifactorial conundrum.

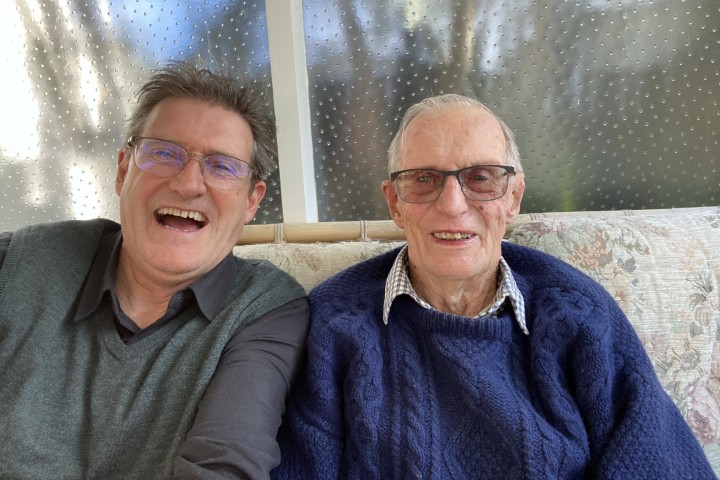
Dr Simon Dean is a consultant ophthalmologist and specialist oculoplastic surgeon at Re:Vision Laser and Cataract Sight Correction Centre and Te Whatu Ora Counties Manukau, Auckland.